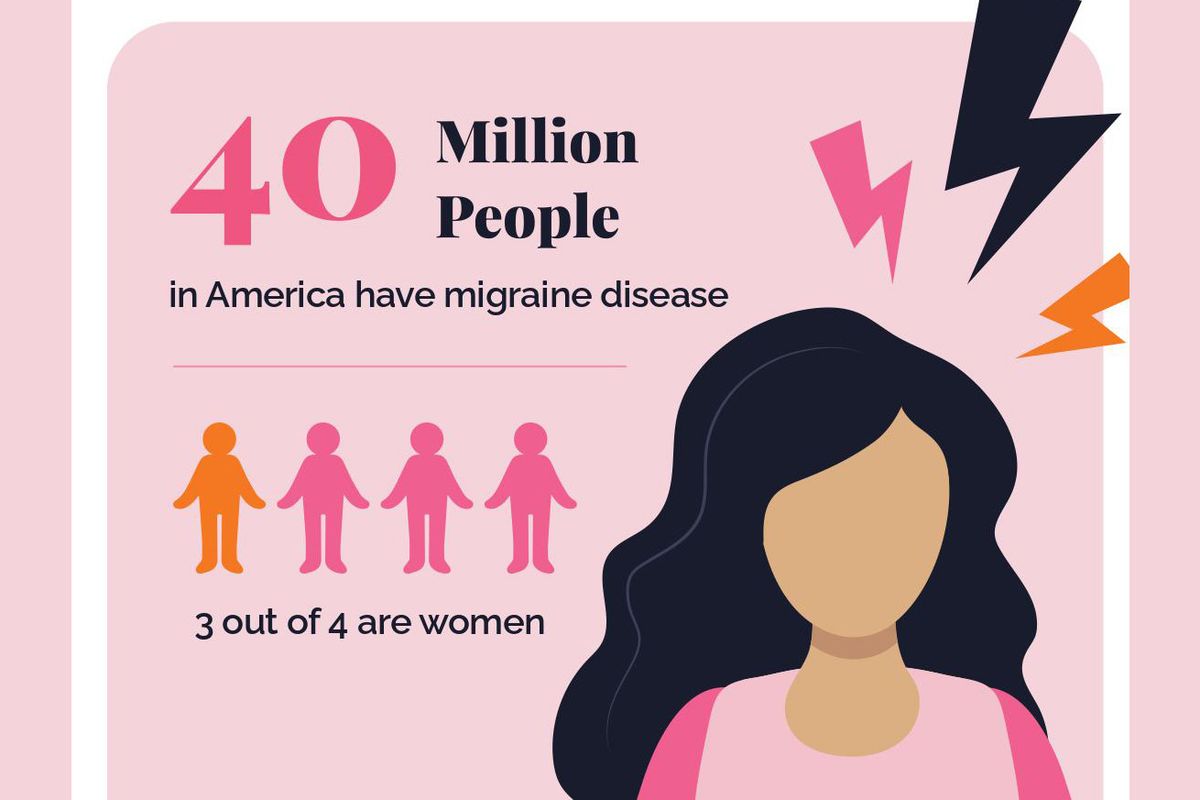
The stabbing blow of a migraine attack is often compared to having an icepick thrust between the eyes. Of the more than 29.5 million people in America who live with the debilitating, painful symptoms of migraine disease, about three out of four of them are women.
Understanding the sex differences in migraine disease is important. Ninety percent of people are unable to work or function normally during their migraine, and women, who work nearly an hour longer per day than men, assume the brunt of paid and unpaid labor while experiencing the lion’s share of migraine pain. And in case you were wondering, a bad migraine can feel worse than childbirth. Therefore, it’s not a stretch to say that for many women, dealing with migraine pain while going about their daily lives is worse than asking them to make dinner as they’re pushing out a baby in the delivery room.
We don’t fully understand what causes migraine, which means there is no absolute cure for the disease. But exploring the sex differences in migraine may help some women learn more about their symptoms, various treatment options and how the disease impacts periods, menopause, birth control, even pregnancy.
What are some of the sex differences experienced by men and women who suffer from migraine?
Before puberty, more boys than girls get migraine. The tables start to turn after puberty, when migraine disease becomes more common in teens and adult women.
Women and men experience some similar migraine issues because of changing levels of serotonin, which is a chemical produced in the brain and the gut that helps nerve cells communicate. A protein called calcitonin gene-related peptide (CGRP) also appears to be involved in migraine symptoms by increasing inflammation and pain in the nervous system. Only women, however, experience migraines due to fluctuations of the hormone estrogen, which is important for sexual and reproductive development.
During their reproductive years, women experience more migraine attacks. It’s suspected that the culprit for these increased migraine attacks is estrogen. Many women report getting a migraine a day or two before getting their period (when estrogen levels are lower than at other times of the month), as well as on the first three days of bleeding.
Many women experience longer migraine attacks than men, as well as increased frequency of nausea, vomiting, dizziness and vertigo, intolerance to certain odors and allodynia, which is a heightened sensitivity to things that aren’t usually painful, like bed linens lightly touching the skin. Women also have fewer periods of remission (when they are symptom-free for prolonged periods of time) than men.
Pregnancy and menopause
Pregnancy may impact a woman’s migraine symptoms. Between 50% and 80% of women who had migraine before pregnancy experience a reduction in their symptoms, but some women without a history of migraine attacks actually get them for the first time when they are pregnant. It’s important to speak with a health care provider to learn how migraine may impact a pregnancy and whether it’s safe to take medication. The same goes for women who are breastfeeding, as some medications can be passed to infants through breast milk.
During perimenopause (the period of time leading up to menopause), migraine attacks may become more severe or frequent due to big fluctuations in hormone levels. The good news is that most women get far fewer migraine attacks after menopause — some women stop getting them entirely.
Treatment options
Some migraine treatments are the same for all sexes. Pain relief such as ibuprofen, naproxen sodium and acetaminophen can help take the edge off, while triptans are a class of prescribed oral medications that target serotonin receptors. Overuse of these popular medicines may cause “rebound headaches,” now renamed medication overuse headache or MOH. This is the term used to describe the phenomenon when migraine attacks become more frequent over time when as needed medications are being used too frequently. In general, using as needed pain medications more than 2-3 days per week can increase the risk of migraine becoming more frequent over time
In 2018, a new type of treatment that helps create antibodies against CGRP was approved by the FDA. Botox shots (yes, the same injections that are used to decrease wrinkles) are also approved for chronic migraine (defined by having headaches more than 15 days per month), and a slew of non-drug options may be tried to prevent or decrease symptoms. Women may also want to learn the things that trigger their migraine (food, stress, and lack of sleep, for example) and then actively work to avoid those triggers.
Some hormonal birth control options may decrease the severity or frequency of migraine attacks. Yet women living with migraine should speak with a health care provider before taking hormonal birth control options, as some of them may increase the risk of stroke and cardiovascular disease. Additionally, women who experience migraine with aura (visual disturbances, numbness, weakness or difficulty speaking) may increase their risk of deep vein thrombosis (DVT; blood clots) by taking hormonal birth control.
If you’re interested in learning more about migraine management, speak with your health care provider and visit HealthyWomen.org.
- Botox and Migraine: What You Need to Know - HealthyWomen ›
- The Migraine Treatment You Don't—But Should—Know About - HealthyWomen ›
- Everything You Need to Know About Migraine Disease - HealthyWomen ›
- Healing Environments Need to Recognize Migraine Triggers - HealthyWomen ›
- I Finally Figured Out What Was Causing My Migraines - HealthyWomen ›
- A New Device Can Help Healthcare Providers Treat Migraine Attacks - HealthyWomen ›
- Questions and Answers About Migraine Disease - HealthyWomen ›
- I Can't “Push Through the Pain” with a Migraine - HealthyWomen ›
- Migraine Toolkit - HealthyWomen ›
- Guía práctica para migrañas - HealthyWomen ›