September is National Atrial Fibrillation (AFib) Awareness Month
Cardiovascular disease (CVD) is the number one cause of death in women in the U.S. But only 44 out of 100 women know that CVD is their biggest risk. Knowing the signs and symptoms of CVD and when to talk to your healthcare provider (HCP) can save your life.
What is cardiovascular disease?
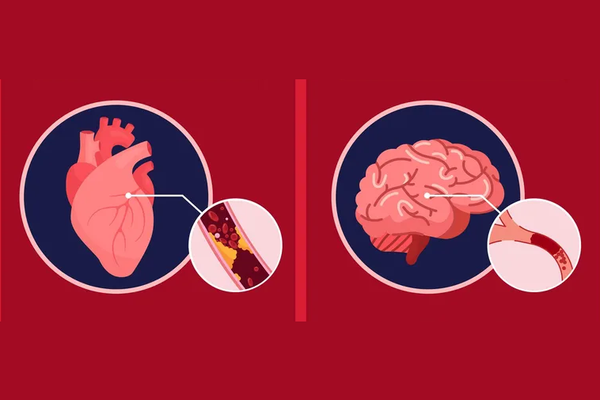
CVD includes any disease that affects the heart or blood vessels. There are many different types of CVD, but some of the types that affect women the most are coronary artery disease, arrhythmia and stroke.
- Coronary artery disease (also known as coronary heart disease) is the leading cause of death in women. It’s also the most common type of heart disease and is caused by a buildup of plaque in the walls of coronary arteries, the tube-like vessels that bring blood to the heart.
- Arrhythmia is when the heart beats irregularly, meaning it’s either beating too slow or too fast or in another abnormal way. The most common type of arrhythmia is atrial fibrillation (AFib), when irregular beating in the upper chambers of the heart make it difficult for blood to flow to the lower chambers.
- Stroke is when a burst or blocked blood vessel stops blood flow to the brain, causing the brain cells to die. There are many different types of stroke, but 8 out of 10 strokes are preventable.
How common is cardiovascular disease?
CVD is very common, especially in women. Almost 1 in 2 women over the age of 20 are living with some type of CVD, and about 1 out of 16 women in that age group have coronary heart disease.
Women are at a higher risk of developing AFib than men. In fact, 1 in 4 women will develop AFib in their lifetime, and the risk increases with age. AFib increases a person’s risk of stroke, which is the third leading cause of death in women in the U.S., affecting 1 out of 5 women ages 55 to 75. People with AFib have a five times greater risk of having an ischemic stroke. Among all races, Black women have the highest rates of stroke.
What are the risk factors for developing cardiovascular disease?
Prevention is key when it comes to reducing your risk of CVD. Some factors that may increase your risk include:
- High blood pressure
- High cholesterol
- Smoking
- Diabetes
- Having overweight or obesity
- Eating an unhealthy diet
- Not getting enough exercise
- Drinking too much alcohol
- Stress and depression
The female reproductive system also adds additional risk factors that men don’t have:
- Getting your first period before the age of 11
- Going through menopause before the age of 40
- Having polycystic ovary syndrome (PCOS)
- Experiencing certain pregnancy complications:
- Gestational diabetes (diabetes during pregnancy)
- Preterm delivery or delivering a baby with low or high birth weight
- Hypertensive disorders of pregnancy, such as preeclampsia and hypertension of pregnancy
CVD is the number one cause of death in new moms.
What are the symptoms of cardiovascular disease I should be aware of?
The symptoms of CVD look different in women than men, so it’s important to know what to look out for and when to contact your HCP.
For coronary artery disease, having a heart attack is often the first sign. As with men, the most common heart attack symptom in women is chest pain or discomfort. But in women, signs of having a heart attack may not be obvious. They may experience other symptoms that are typically less associated with heart attack, such as shortness of breath, nausea/vomiting and back or jaw pain.
According to the American Heart Association, call 911 if you have any of these symptoms:
- Uncomfortable pressure, squeezing, fullness or pain in the center of your chest that lasts more than a few minutes, or goes away and comes back.
- Pain or discomfort in one or both arms, the back, neck, jaw or stomach.
- Shortness of breath with or without chest discomfort.
- Breaking out in a cold sweat, nausea or lightheadedness.
Read: Symptoms of Heart Attacks in Women >>
Symptoms for AFib might include:
- Racing heart
- Heart palpitations (a feeling that your heart is fluttering or skipping a beat)
- Shortness of breath
- Chest pain
For women, feeling weakness or fatigue is an additional symptom to be aware of. It’s also common for women to experience any of these symptoms more often or for longer periods of time than men.
Stroke symptoms can come on quickly. Using the American Stroke Association’s acronym F.A.S.T. can help you remember what symptoms to look out for:
F = Face Drooping – Does one side of the face droop or is it numb? Ask the person to smile. Is the person's smile uneven?
A = Arm Weakness – Is one arm weak or numb? Ask the person to raise both arms. Does one arm drift downward?
S = Speech Difficulty – Is speech slurred?
T = Time to call 911 – Stroke is an emergency. Every minute counts. Call 911 immediately. Note the time when any of the symptoms first appear.
Some other stroke symptoms might include:
- Confusion, trouble speaking or understanding speech
- Difficulty seeing in one or both eyes
- Difficulty walking, dizziness, loss of balance or coordination
- Severe headache with no known cause
What if my healthcare provider dismisses my symptoms?
There is a misconception, even among some HCPs, that women develop CVD at much lower rates than men. One study found that both gender bias and biological differences between men and women may be to blame for the differences in diagnosis and treatment of CVD in women.
Read: Why Don’t Women Get the Same Treatment for Heart Disease as Men? >>
If you experience any symptoms of CVD, talk to your HCP right away. Be clear and direct about what symptoms you’re having, how much pain or discomfort they cause you, how long you’ve had them, and how often you experience them.
If your provider dismisses your symptoms or you don’t feel heard by them, you have the right to get a second opinion from another provider. Ask if you can be referred to a cardiovascular specialist or find a new provider in the same or different practice.
When it comes to your cardiovascular health, don’t wait.
This educational resource was created with support from BMS.
- Clinically Speaking: Questions to Ask Your HCP About Cardiovascular Disease ›
- Symptoms of Heart Attacks in Women ›
- Did You Know That Heart Disease Affects Women of Color Differently? - HealthyWomen ›
- Cardiac Arrest vs. Heart Attack - HealthyWomen ›
- What Is Heart Disease? - HealthyWomen ›
- Are You at Risk for Heart Disease? - HealthyWomen ›
- How to Reduce Your Risk for Stroke - HealthyWomen ›
- List of heart disease resources - HealthyWomen ›