Skeletons don’t get the love they should (spooky season excluded, of course).
But your bones certainly deserve a standing ovation considering everything they do for you.
Your bones have been protecting vital organs and supporting your body since you were in your fetus era. And they act as a storage bank for calcium, which your body needs for healthy cells and bones.
But age-related bone loss and factors like poor nutrition and lack of physical activity can lead to bone conditions later in age, including:
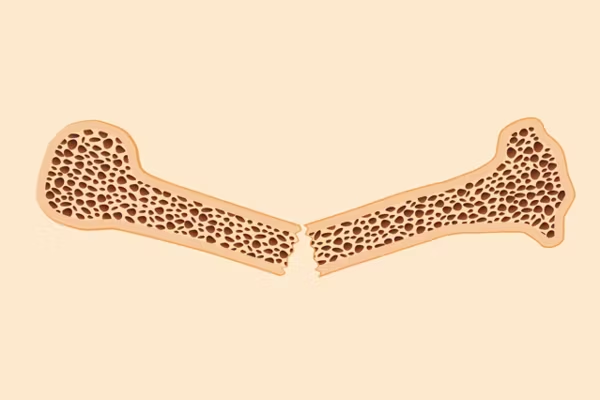
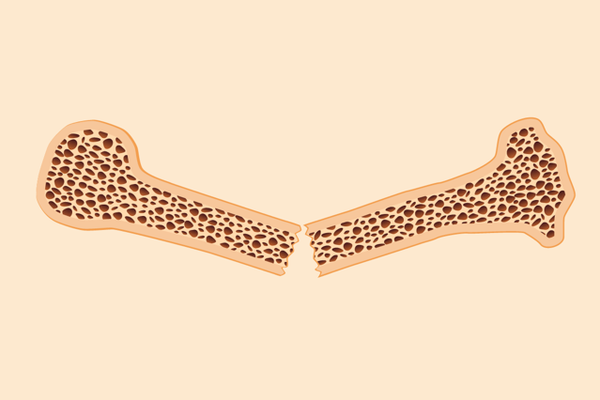
- Osteopenia: A condition where bone mass density is lower than it should be, leaving bones vulnerable to breaks
- Osteoporosis: A disease that weakens the bones and increases the risk for serious broken bones
Read: Questions to Ask Your Healthcare Provider About Bone Health >>
Bone health throughout the years
Bone density and strength increases throughout childhood and as a young adult, but time is limited for influencing peak bone mass for optimal bone health.
Here’s a look at the importance of women's bone health at key stages of life.
- Birth through to pre-puberty
From the time you’re a tiny baby into adolescence, your bones go through an important process called modeling.
During this time, your body forms new bone in existing bone that grows with your body and also helps bones shift into place where they should be.
Bone mass grows slowly in the beginning, and then doubles during puberty. In order to grow strong bones, you need to get the proper amount of calcium and vitamin D through food sources rich in these nutrients, fortified foods or supplements. The recommended amount of vitamin D and calcium per day varies based on age:
- Vitamin D:
- Infants younger than 12 months: 400 international units (IU)
- Children and adolescents: 600 IU
- Calcium
- 6 months and younger: 200 mg
- 7–12 months: 260 mg
- Children and adolescents:700-1,300 mg
Deficiencies in vitamin D and calcium can affect bone health and cause a bone-softening disease called rickets. Not getting enough of these nutrients also increases the risk for broken bones throughout childhood and into adulthood, among other problems.
- Puberty to young adulthood
The teen years are admittedly awkward but also very cool for bone health.
From puberty into young adulthood, you’re continuing to build and strengthen bones, which can help keep osteoporosis at bay later in life.
Think of your bones like a savings account: Developing good bone health at an early age means you’ll have enough to spare when natural bone loss starts to happen in midlife.
Factors that can affect bone health can include:
- The age you start puberty: Research shows early onset of puberty is associated with higher bone mass density and strength. But a delayed onset of puberty (after age 12) has been linked to a higher risk of osteoporosis later in life.
- Your period: Irregular or missed periods (amenorrhea) may lead to lower bone density. And the age you start your period may also affect bone health. One study of postmenopausal women found participants who started their period after 16 had a higher risk of fractures of the lower spine caused by osteoporosis.
- Having an eating disorder: Nutritional deficiencies caused by anorexia and bulimia can make your bones weak and cause amenorrhea, which can also weaken bones.
Eating a diet rich in calcium and vitamin D is important for bone health. For women up to age 50, that means 400-800 IU a day of vitamin D and 1,000 mg of calcium.
Weight-bearing exercises such as jogging and hiking are also key for bone density, structure and strength. Weight bearing means any activity that uses your own body weight, so even walking as exercise and jumping help increase and maintain bone strength. Resistance training with weights or using your own body weight is also recommended for bone health at least two days a week.
Read: 6 Ways to Strengthen Your Musculoskeletal System >>
- Early 20s to 30
By the time you’re in your early 20s, your bones have reached their maximum strength and density, also known as peak bone mass (PBM). Basically, all the bone strength and growth you’ve done over the years leads up to your PBM.
Your bones still go through the process of remodeling, just not at the same rate as when you were younger. But outside factors like nutrition and exercise can help maintain and build bone strength.
Calcium is especially important for people who are planning a pregnancy. The amount of calcium you need doesn’t change during pregnancy, but if there’s not enough calcium for the baby, it will be taken out of your bones.
Calcium is also important when breastfeeding because the same thing can happen — your body will take calcium from your bones for the breastmilk.
The good news is that any bone loss during pregnancy and breastfeeding is usually temporary.
Kids or no kids, everyone starts to lose slightly more bone mass than you gain around the age of 30.
Hormone levels fluctuate in the time leading up to menopause (perimenopause). As estrogen levels start to decline, so does the protection for your bone density. This makes your bones more vulnerable to fractures and osteoporosis.
Weight-bearing exercises and strength training are crucial to keeping bones as healthy as possible and preventing the risk for fractures and osteoporosis. Of course, nutrition plays a big role. Your body doesn’t make calcium, so you have to get it from food or supplements. And vitamin D helps the body absorb calcium.
Women over 50 should get 1,200 mg of calcium and 600 IU of vitamin D a day.
What you can do to prevent falls and fractures
In addition to nutrition and physical activity, there are other things you can do to reduce your risk for injuries and broken bones.
- Keep your home clutter-free and remove any objects that you might trip over.
- Add support bars and railings in the bathroom and around stairs.
- Make sure there’s enough light in your rooms.
Talk to your healthcare provider about your risk for falling and whether you should be screened for osteoporosis. The Bone Health and Osteoporosis Foundation recommends all women 65 and older get screened for osteoporosis. Postmenopausal women younger than 65 with one or more risk factors in addition to being postmenopausal (low body weight, family history of hip fracture, smoking, drinking alcohol, etc.) and anyone who has experienced a fracture after age 50 should also be screened.
If you’ve been diagnosed with osteopenia or osteoporosis or have had a fracture, talk to your HCP about what you can do to decrease the risk for future bone problems.
Good bone health for life
Although your early years are crucial for influencing peak bone mass and decreasing your risk for osteoporosis, you can maintain and even increase bone strength at any age. It takes work, but it’s never too late to prioritize your bone health.
This educational resource was created with support from Sandoz, a HealthyWomen Corporate Advisory Council member.
- 15 Minutes With: Vonda Wright Talks Bone Health During Menopause and the Secret to Living a Long, Healthy Life ›
- Fast Facts: 10 Facts About Osteoporosis in Women ›
- Clinically Speaking: Questions to Ask Your Healthcare Provider About Osteoporosis ›
- Women and Bone Health Basics ›
- Questions to Ask Your Healthcare Provider About Bone Health ›
- Información acerca del sistema locomotor - HealthyWomen ›