Lee Pearson wasn’t going to let anything postpone the Caribbean summer vacation she and her husband had been planning for years. Even though she’d been seeing blood in her urine for months and had an increased urge to urinate, Pearson, who is Black and was 71 at the time, felt she could wait before contacting a healthcare provider (HCP).
“I said I would check it out when I got back,” Pearson said. “But when we were there, the frequency and urge to urinate became almost unbearable. It nearly ruined the trip.”
Pearson visited her primary care physician a week after she returned. The physician referred her to a urologist, who performed a cystoscopy, or bladder scope, that detected a tumor on her bladder. It was stage 4 bladder cancer.
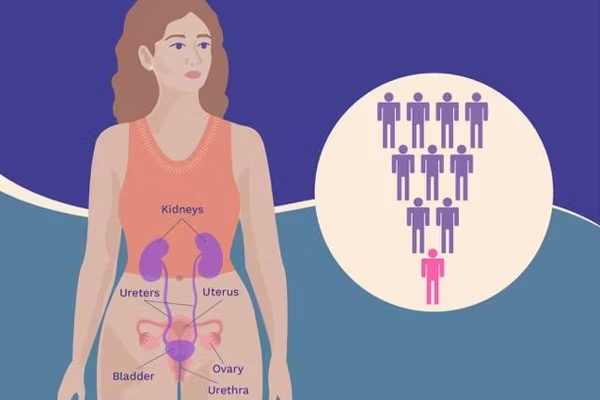
Older adults have a higher risk of developing bladder cancer, a condition that occurs when cancer cells grow in the bladder. Although it can occur at any age, 90% of cases are in people over 55, with 73 being the average age at the time of diagnosis. Risk factors include smoking, a family history of bladder cancer, and inflammation of the urinary tract due to urinary tract infections (UTIs) or sexually transmitted diseases.
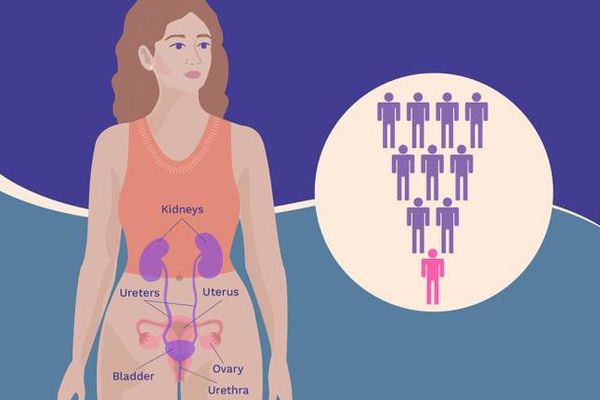
Although women are less likely to develop bladder cancer than men — 19,450 of the 83,730 estimated new bladder cancer cases in 2021 were among women — they can face worse outcomes after diagnosis. African Americans also have lower bladder cancer survival rates despite having fewer new cases than white individuals.
As Pearson began learning more about the disease, she recognized that she had multiple risk factors for developing bladder cancer. In addition to being over 55 when she was diagnosed, Pearson also had two brothers who both died after developing multiple cancers, including bladder cancer.
The bladder cancer burden for Black women
“Bladder cancer is the only cancer where women do worse than men after the diagnosis,” said Dr. Armine K. Smith, director of urologic oncology at the Kimmel Cancer Center at Sibley Memorial Hospital in Washington, D.C, and an assistant professor of urology at the Johns Hopkins University School of Medicine. “Some of that may be related to biology and some of it has to do with women, on average, taking longer to be diagnosed in the first place.”
Because blood in urine is often one of the first presenting symptoms, women accustomed to seeing blood in their urine during menstruation or because of a UTI might not recognize it as a sign of something more serious. Too often, they’re given a prescription for antibiotics and sent home. By the time bladder cancer is diagnosed, it’s reached a more advanced stage.
Men who detect blood in their urine might be more likely to see it as abnormal and tell their HCPs. Smith said more men, especially older men, also have a relationship with a urologist because of past procedures or other conditions, making it easier to get an early bladder cancer diagnosis.
That type of relationship indirectly helped save Pearson’s life. Pearson’s husband is a prostate cancer survivor and had developed a close relationship with the head of the urology clinic where he was treated. When Pearson tried to get an appointment at that clinic, she was told they were booked for weeks. Her husband made a few calls, and she was able to see a urologist the next day.
While Pearson’s personal connections and physical location, which happens to be close to top urology and oncology specialists in the Baltimore area, helped increase her chances of long-term survival, later diagnoses, less aggressive treatment and a lack of access to quality care are often cited as contributing factors to lower survival rates for Black bladder cancer patients.
“There’s also one specific type of cancer — adenocarcinoma of the bladder — that’s a little bit more prevalent in African Americans and usually arises in the lower portion of the bladder,” Smith said. “Whether it’s an anatomical or hormonal difference, we don’t know, but we do see that African American women are more predisposed to this cancer.”
Nearly all adenocarcinomas are invasive, meaning that the cancer has moved into the bladder wall or outside the bladder, and requires aggressive treatment.
The hollow shape of the bladder makes bladder cancer difficult to treat. The urothelial cells in the epithelial lining of the bladder also cover the tubes that lead to the kidneys, putting a larger area at risk of cancer spread and making it more difficult to cut out the cancerous cells. This is a major reason why bladder cancer has a high likelihood of recurrence.
“I tell my patients we’re going to be friends because I’m going to be seeing them a lot,” Smith said. “The average surveillance is five to 10 years for these conditions because so many times, you treat it and it comes right back.”
A second chance after bladder cancer
Between her urologist, bladder cancer specialist, husband and even a savvy 16-year-old granddaughter who researched bladder cancer and treatment on the internet, Pearson had a strong team helping her through the process.
She began chemotherapy that fall to shrink the tumor and underwent surgery to remove it the following February. A cystectomy was also performed to remove all reproductive organs to prevent cancer cells from spreading.
Pearson spent a week in the hospital after her wound became infected, but while she was there, her oncologist gave her the most positive news she’d heard in six months: She was cancer-free.
“That was March 3, 2016,” she said. “And here I am, more than five years later, still cancer-free.”
Now 76, Pearson works to raise awareness about bladder cancer through organizations like the Bladder Cancer Advocacy Network (BCAN) and volunteered at a hospital before the Covid-19 pandemic. She sees her HCPs frequently and has grown accustomed to living with an ostomy, which allows waste to pass into a pouch outside her body.
Pearson often thinks about the friends and family, including two brothers, she lost to bladder cancer and feels grateful for the chance to spend more years with her husband, daughter, three grandchildren and three great-grandchildren.
“When I heard I was in stage 4, I didn’t think they were going to be able to do anything for me, but God put me in the right hands,” Pearson said. “And thank God, I got through it.”
This resource was created with joint support from Astellas and Seagen.
- It Took 2 Years and a Second Opinion to Find My Bladder Cancer ... ›
- What Women Need to Know About Urothelial Bladder Cancer ... ›
- It's Bladder Cancer Awareness Month: My Story, Chapter Two ... ›
- A Conversation With Dr. Sarah Psutka About Bladder Cancer ... ›
- Fast Facts: Everything You Need to Know About Urothelial Bladder ... ›
- Bladder Cancer and Black Women - HealthyWomen ›
- El cáncer de vejiga y las mujeres de raza negra - HealthyWomen ›
- How to Regain Intimacy When Your Partner Has Bladder Cancer - HealthyWomen ›
- Cómo recuperar la intimidad cuando tu pareja tiene cáncer de vejiga - HealthyWomen ›
- Q&A About Urothelial Bladder Cancer Treatment - HealthyWomen ›
- Preguntas y respuestas relacionadas con el tratamiento contra el cáncer de vejiga urotelial - HealthyWomen ›