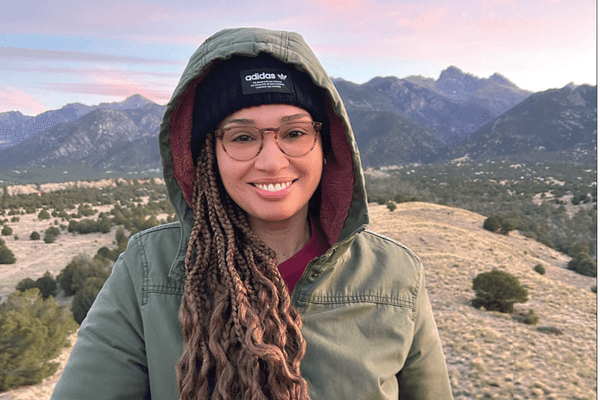
As told to Erica Rimlinger
For 42 years, I’ve been living with complex regional pain syndrome (CRPS), a disorder that causes non-stop intense pain. In that time, I’ve had doctors call me crazy, delusional and a liar. One doctor was so abusive, he told me I should “just shoot myself in the head.” It’s no wonder some people call CRPS the “suicide disease.” Often, the intense, unpredictable pain that left me bedridden for a decade felt like the least of my problems: the major battle was getting the medical profession to believe and treat me.
After enduring years of mistreatment from doctors, I learned to manage my condition using holistic self-care. I didn’t want to enter a doctor’s office ever again unless the need for western medical care was undeniable. That day arrived when I was diagnosed with breast cancer.
When I felt the breast lump in 2018, I waited a year to get it checked. I didn’t trust doctors, who had left me hopeless, abandoned and depressed. But when it didn’t go away and grew larger, I gave in. My first reaction to the diagnosis was shock that I had cancer. My second reaction was dread that I had to re-enter the western healthcare system. Twenty years before, I had been diagnosed with ductal carcinoma in situ (DCIS) in my other breast, and my medical team told me I only had months to live unless I underwent aggressive treatment. I correctly suspected my doctors would not consider my CRPS and that my body could not handle their regimen. I did my own research and learned that most DCIS doesn’t become invasive, and overtreatment was common. I refused their treatment options.
Now that I was diagnosed with stage 2B triple negative breast cancer, I took six months to decide what treatment would be best. The standard plan of chemotherapy, surgery and radiation gave me an impossible needle to thread. The healthcare system didn’t take my CRPS seriously, but I knew surgery and radiation would cause nerve damage, spiking my pain to an intolerable level. And I feared it would never simmer down.

I decided to go with chemotherapy only because I didn’t want to lose the use of the upper right side of my body. As expected, I was verbally abused for thinking outside the box. One doctor told me, “My other patients WANT to live.” I wanted to live just as much as they did. But I wanted quality of life. I’d lived without it and couldn’t go back there. I’d been battling for my quality of life for decades.
As it turned out, my tumor was a “ super-responder” to chemotherapy, disappearing completely by imaging standards. I continued to get monitored and use my self-care techniques, which included exercise, good sleep habits and careful nutrition.
Eighteen months later, my oncologist found a cancerous lump in my right lymph node that quickly grew to the size of a golf ball. After hearing his treatment plan for my recurrence, I hung up the phone and started screaming in fear and frustration.
He'd recommended eight rounds of chemo, followed by a new immunotherapy treatment that had recently become available. After that, he recommended I undergo surgery, radiation and more immunotherapy. After careful consideration and much research, I consented only to low-dose oral chemo and immunotherapy.
The chemo shrank the tumor a little bit, but then stopped working. I was horrified to learn my insurance company wouldn’t cover the immunotherapy because I hadn’t agreed to surgery. I felt I was being punished for making my own treatment choices.
I quickly learned about and was going to try a procedure called cryoablation, a technique that freezes the tumor instead of removing it surgically, which I prayed would avoid triggering my CRPS. Then a blessed event happened — the company that made the immunotherapy treatment had a compassionate care program that allowed me to get the immunotherapy.
After one immunotherapy treatment, my tumor disappeared. My doctors were stunned. There was no need for cryoablation as there was nothing left to cryoablate. I was called a “miracle.”
Looking back from a distance of two years, I wonder if “miracle” is the right term for what happened to me. Am I a miracle, or did I simply make a series of thoughtful decisions that were right for me?
This is not to say immunotherapy was easy. I was hospitalized for colitis and later developed reactive arthritis. It also spiked my CRPS, but to a tolerable level. Bottom line, immunotherapy cured me without destroying my quality of life.
I’m grateful that years of self-advocacy made me strong enough to stand my ground with the doctors who talked to me as though I was a child. I’m also grateful I eventually found a team of four doctors that listened to me, believed in CRPS, and embraced the reality that surgery and radiation would destroy my life.

Best of all, this team worked together, consulting about my care with one another, my life partner, John, and me. Being part of a shared decision-making team that valued individualized care was such a powerful experience, I regained some trust in the medical system. I’m a strong believer that a doctor who isn’t threatened by other opinions is the sign of a true healer.
Sadly, when we are diagnosed with cancer, we tend to panic and blindly put our care into our doctors’ hands. However well-intentioned they may be, we’re the ones who must live (or die) with the consequences of their treatment choices. For the best wellness outcome, I believe we must take responsibility for our own care, and that includes self-care practices to make our bodies healthy enough to make the best of the treatments we choose. I’m certain I’m still here today because I followed my gut.
These days, I eat a healthy, cancer-fighting diet full of fish, berries, nuts and leafy greens. I’m an avid lap swimmer, and I make plenty of time for cuddles with my kitties. I meditate and pray every day, while working on releasing past traumas that have driven my illnesses. I’ve become better at forgiving the people who have harmed and abandoned me.
Also, I engage in meaningful, creative work. I continue to run the nonprofit I founded 22 years ago to help other women in pain. And I’m rekindling past passions. I spent my childhood training for a career as a performer, but as a part-time wheelchair user with CRPS, Hollywood’s doors have been closed to me. After fighting for my life twice, that’s no longer stopping me. I recently got a top-end agent and am already getting great auditions and call-backs for acting and singing roles. Yes, I’m doing it my way.
I look forward to hitting my third cancer-free year, which my team tells me is the goal line for a cure. Until then, I’ll continue to trust myself with my health and happiness.
This educational resource was created with support from Merck
Have a Real Women, Real Stories of your own you want to share? Let us know.
Our Real Women, Real Stories are the authentic experiences of real-life women. The views, opinions and experiences shared in these stories are not endorsed by HealthyWomen and do not necessarily reflect the official policy or position of HealthyWomen.
- Metastatic Breast Cancer Treatment Was Destroying My Spirit — Until I Tapped Into My Colombian Roots and Alternative Medicine ›
- Supporting a Friend Who Has Breast Cancer ›
- Culture Shock, Then a Cancer Shock, Inspired Me to Create the Community I Needed ›
- After I Was Diagnosed with Triple Negative Breast Cancer, I Had Another Shock ›
- I Was Searching for a Miracle Cure for My Breast Cancer. I Found Hope Instead. ›
- How I Got My Sexual Groove Back After Surviving Breast Cancer ›
- My Mom, My Sister and I All Have a BRCA2 Gene Mutation - HealthyWomen ›
- Mi mamá, mi hermana y yo tenemos una mutación genética BRCA2 - HealthyWomen ›
- My “Small” Cancer Turned Out to Be Stage 4 Breast Cancer - HealthyWomen ›
- Facts About DCIS - HealthyWomen ›
- Don’t Count Me Out Because I Have Metastatic Breast Cancer - HealthyWomen ›
- Información comprobada del CDIS - HealthyWomen ›