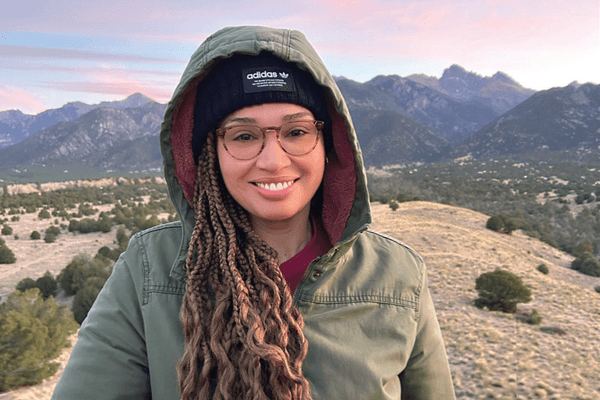
When I learned my triple-negative breast cancer had spread into my chest wall, a tidal wave of shock and disbelief crashed over me. As the wave receded, anxiety rolled in. I focused on my survival odds, which I recited to my oncologist: "Fifteen percent without treatment, 50% with treatment."
My doctor encouraged me to use the hospital's resources to help manage my fear and anxiety, but I was convinced I didn't need them and regularly dodged my hospital's breast cancer care coordinator, Susan, and her support-group brochures.
Maybe I could have coped on my own, if fear and anxiety had been the only emotions that required processing, but they formed just the base layer of complex emotional issues that piled up over the next 12 months and beyond.
Fear, anxiety and despair
"Cancer exacts an emotional toll on you and your entire social ecosystem," said Dr. Barbara L. Andersen, professor of psychology at Ohio State University. This is especially true, she said, in the period that immediately follows diagnosis, before test results have come back to form a clear picture of the treatment plan.
The fear and despair that breast cancer patients feel can be intense and can put them at risk for depression.
"When mood is low, there is a loss of enjoyment in life or motivation, loss of appetite, sleep difficulties, and other issues. Forcing yourself to 'be positive' is not going to fix that," Andersen said. "Staying positive doesn't cure depression, treatment does." Moreover, healthcare providers, family or friends advising patients to "be positive" may make them feel guilty for their feelings of despair.
"A trained professional can help," said Andersen.
Stress and its impact on physical health
Like asking the '"chicken or the egg" question, it's hard to tell whether the physical impacts of breast cancer treatment — the feelings of fatigue, pain and nausea — are made worse by emotional stress, or if emotional stress is made worse by the side effects of treatment. Either way, research has shown a clear link between the two.
Andersen has spent her career collecting a body of research linking stress management in cancer patients to better immune responses. In one study, breast cancer patients who spent 12 months taking part in a support group had significantly less emotional distress, improved social relationships, improved diet changes, and coped better overall. After 15 years, the women who participated in the intervention showed a 45% reduction in risk of recurrence compared to the women in the control group.
"Even when intervention was long over," said Andersen, "women who received that higher social support had higher levels of immunity. They lived, on average, 18 months longer [than women in the control group]."
Krista Park Berry, director of the Susan G. Komen Breast Care Helpline, agreed that group and individual support can help women cope. She also noted that complementary therapies can reduce stress and help relieve side effects.
"Many people use complementary and integrative therapies, such as acupuncture, prayer and mindfulness meditation, during or after their breast cancer care," said Berry. But she cautioned that these treatments should not be used to treat breast cancer itself. "Before you begin a complementary therapy, talk with your healthcare provider to help avoid problems with your breast cancer treatment."
Berry said one such therapy — mindfulness meditation — "uses breathing methods and may include guided imagery, as well as other relaxation and stress-reduction techniques. Some findings show mindfulness meditation can reduce stress, anxiety, fear of recurrence and fatigue in breast cancer survivors, and increase quality of life.
"Prayer and spiritual faith might make some people feel more positive or hopeful. This can support relaxation, reduce anxiety, and lower the effects of stress," said Berry.
Logistical challenges
I found that managing stress is not optional, especially when it's coming at you from all sides. In addition to physical challenges faced by the patient, coping with the realities of breast cancer can contribute to the emotional toll for patients and their families.
For example, as costs related to treatment grow, the ability to work may become an issue. And because our healthcare system relies heavily on employers to provide health insurance, breast cancer patients can be faced with the choice of working full-time through treatment or losing their health coverage.
Interpreting medical bills, checking insurance coverage, arranging appointments, getting to appointments and making sure the rest of your life is covered while you're at appointments can be complicated and time-consuming. I was fortunate to have decent health insurance that remained uninterrupted during treatment, but even in my situation, dealing with health insurance and medical bills felt overwhelming.
Cancer doesn’t affect only you
As with any major illness, breast cancer can have far-reaching effects beyond the person who is diagnosed. Spouses, partners, family members and loved ones may feel many of the same emotions as the person diagnosed: shock, sadness, fear, anger and denial.
Loved ones want to help, and allowing them to help ease some of the burdens of treatment, such as getting to appointments, arranging childcare and shopping for groceries, may help you -— and them — feel less powerless over the situation. My husband took comfort in untangling health insurance issues and found that it even helped relieve his own stress. When I asked him why he didn't mind arguing (politely, of course) with the health insurance service reps, he told me, "I feel like this is the one thing I'm actually able to do to help you."
If you have children, they may have a strong emotional response to a parent's breast cancer diagnosis. Berry advised telling children about the diagnosis in a way suited to their age and state of mind. "If they aren't told by an adult, children may fill in the gaps with their imagination," Berry said. "Be watchful for signs of emotional distress, both at home and at school." She recommended involving children in family discussions and decision-making related to a parent's breast cancer and making children feel comfortable asking questions and sharing emotions.
I allowed my son, a fourth grader at the time of my second diagnosis, to shave my hair. He gave me a mohawk, and neither of us could stop giggling. The fiasco turned a day I'd once dreaded into a game and a fun family memory we still recall with laughter.
Find your resources
Resources are available both locally and nationally to help cope with breast cancer. Ask your healthcare provider if your hospital has support services or connections to local or national support groups or services.
Suzanne Brace, executive director of the Hopewell Cancer Center in Baltimore County, MD, meets with newly diagnosed patients who come to Hopewell for support groups, exercise, and meditation classes and education. She said she fields a huge range of questions that include, "Will I lose my job? What shall I tell my kids? How do I handle this? What information is safe to say to my employer? How do I know I'm getting the right treatment?"
All of these questions, she said, are normal and generated by the immediate shock of diagnosis. Essentially, she said, people are processing a new reality where they don't know what the future holds. "They're saying: 'My life just changed and it won't ever be the same.'"
Later, when your cancer journey is further behind you, you might want to speak with or support someone who is just embarking on this stressful, involuntary roller-coaster ride. If and when that time comes, Brace said, you can help someone else normalize the experience of living with a cancer diagnosis.
"Sometimes all it takes is meeting someone who can say, 'I've had it, too. But here I am.'"
Resources
The American Cancer Society
Susan G. Komen Tools & Resources
BreastCancer.org
This resource was created with support from Daiichi Sankyo and Merck.
- Life After a Breast Cancer Diagnosis ›
- Olivia Munn’s Breast Cancer Diagnosis Is a Wake-Up Call for All Women ›
- Overcoming the Fear of Breast Cancer ›
- My Life Really Began When I Got My Breast Cancer Diagnosis ›
- Questions to Ask After a Breast Cancer Diagnosis - HealthyWomen ›
- Advanced Breast Cancer: Provider's Perspective - HealthyWomen ›
- I Have Outlived My Metastatic Breast Cancer Diagnosis - HealthyWomen ›
- Superé las expectativas de vida de mi diagnóstico de cáncer mamario metastásico - HealthyWomen ›