The statistics may surprise you: Lung cancer kills more women in the U.S. than any other cancer.
About 120,000 women are diagnosed with lung cancer each year and about 60,000 women die from the disease. Although lung cancer is commonly associated with smoking, it’s important to know that non-smokers can get lung cancer, too.
Here’s what you need to know about the different types of lung cancer and how they’re treated.
There are three types of lung cancer with many subtypes
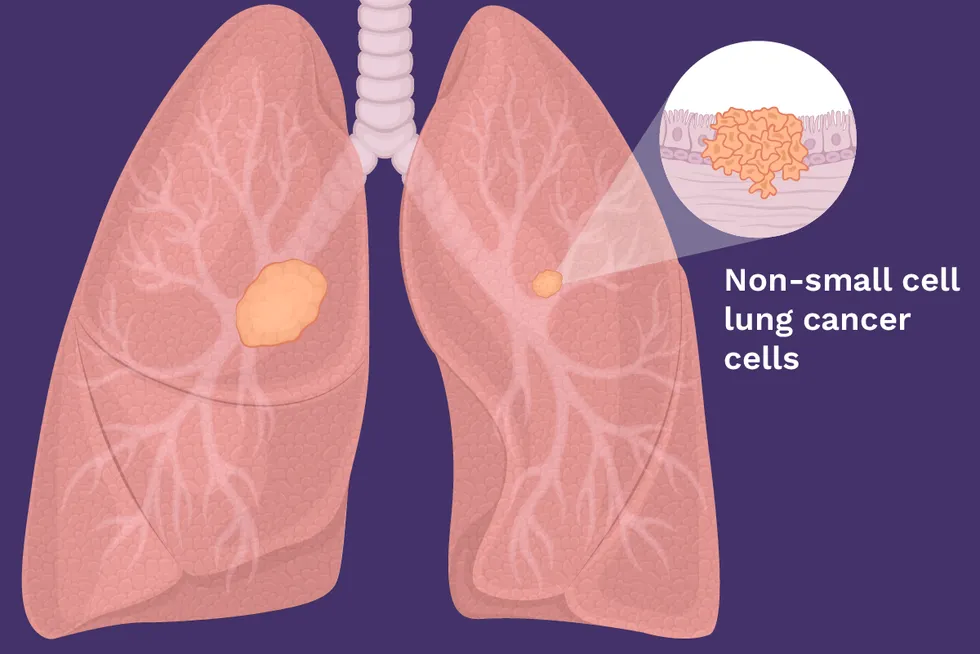
1. Non-small cell lung cancer (NSCLC)
Non-small cell lung cancer (NSCLC) makes up 85 out of 100 of all lung cancer cases. Its main subtypes start from different types of lung cells, but the treatment options are often similar, so healthcare providers (HCPs) often group them together.
The main types of non-small cell lung cancer are:
Adenocarcinoma
- Grows from mucus-producing cells in the outer parts of the lung, which makes it more likely to be diagnosed early
- Makes up about 4 out of 10 NSCLC cases
- Is more common in women and younger people who develop lung cancer, including people who don’t smoke
Squamous cell carcinoma
- Tumors start in the squamous cells, which line the inside of the lung’s airways
- Makes up about 3 out of 10 NSCLC cases
- Usually develops in people with a history of smoking
- Often located near the center of the chest, which can make them hard to treat
Large cell carcinoma
- Can grow in any part of the lung
- Make up about 1 out of 10 cases of lung cancer
- Tends to grow and spread quickly
Other rare NSLC subtypes
- Large cell neuroendocrine carcinoma
- Adenosquamous carcinoma
- Sarcomatoid carcinoma
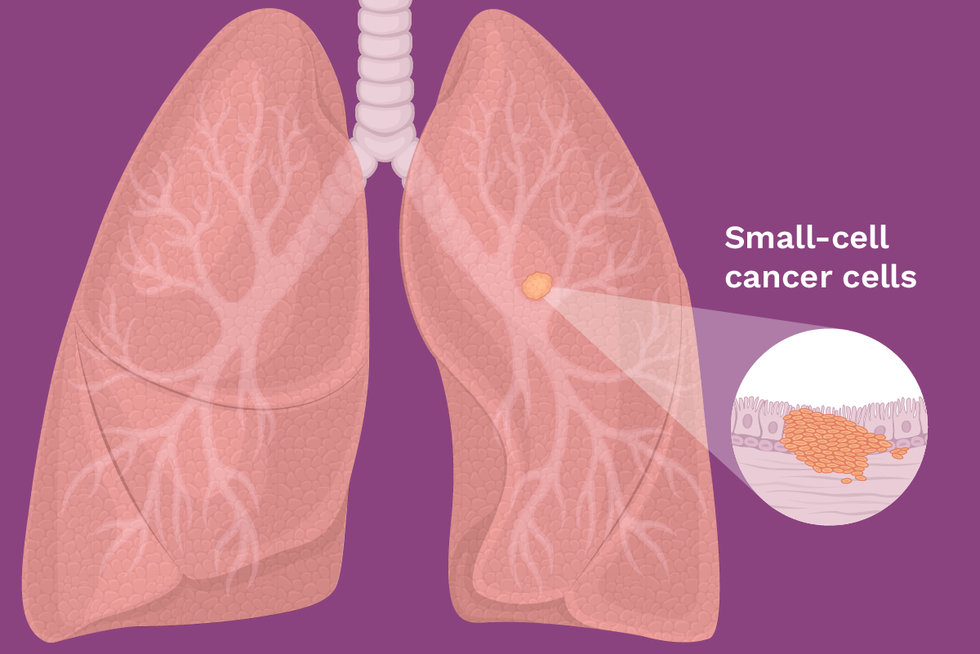
2. Small cell lung cancer (SCLC)
Small cell lung cancer (SCLC) is the other major type of lung cancer. The name comes from the way the cells look under a microscope: they’re smaller than the cells seen in NSCLC. About 10–15 out of 100 cases of lung cancer are SCLC, which is sometimes called oat cell cancer.
SCLC is the most aggressive type of lung cancer and usually diagnosed at an advanced stage.
3. Lung carcinoid tumors
Lung carcinoid tumors grow in the lung’s neuroendocrine cells, which perform functions like controlling air and blood flow in the lungs or adapting to differing oxygen levels in the air we breathe. There are two types of lung carcinoid tumors: typical and atypical.
- Lung carcinoid tumors are rare and usually slow growing.
- Typical carcinoid tumors make up about 9 out of 10 lung carcinoids.
- Atypical lung carcinoids tend to grow faster and are more aggressive.

Lung cancer treatment options
If your HCP thinks you have lung cancer, it’s important to get the right diagnosis. That’s because your lung cancer treatment will be based on the specific type and stage of lung cancer you have.
Treatment plans for lung cancer typically include surgery, radiation therapy and chemotherapy. Your HCP may also recommend immunotherapy or — if your tumor contains genetic mutations or alterations — targeted therapy.
To learn about different treatment options for lung cancer, you can use the American Lung Association’s Lung Cancer Treatment Planning Tool. It includes a decision-making worksheet you can download to use when talking to your HCPs.
Biomarker testing
About 4 out of 10 people with NSCLC are diagnosed with stage 4 disease, the most advanced type.
According to National Comprehensive Cancer Network (NCCN) guidelines, all patients with newly diagnosed stage 4 NSCLC should receive testing for lung cancer biomarkers. These chemical signatures can indicate whether your tumor has a genetic mutation, meaning that changes in its DNA might have led to you developing cancer. If so, your doctor can use a targeted therapy designed for that mutation to fight your cancer.
Genetic mutations that can contribute to lung cancer growth often occur on one or more of these genes, including:
- EGFR
- ALK
- KRAS
- BRAF
- HER2
- ROS1
- RET
- MET
- NTRK
- STK11
Your doctor may recommend other types of testing, including:
- PD-L1 Testing: No matter what type or stage of lung cancer you have, your doctor may also recommend testing your tumor for PD-L1. This is a protein found on the surface of some cancer cells, and it stops the body’s immune cells from destroying the cancer. Knowing if the tumor has PD-L1 will help your doctor decide if immunotherapy will be effective against your cancer. This testing is not used if you have an EGFR or ALK mutation.
- Tumor Mutational Burden (TMB) Testing: Like PD-L1, TMB is a biomarker that may help tell your doctor whether immunotherapy might be effective against your lung cancer. TMB testing shows the number of mutations inside a tumor. Your immune system must be able to recognize at least one abnormal protein for immunotherapy to work. If you have an EGFR or ALK mutation, you will not receive TMB testing.
- Circulating Tumor DNA: Your doctor may use a blood test known as a liquid biopsy to learn about your cancer. The test collects dead cancer cells from your bloodstream so your doctor can learn about the tumor’s genetic makeup.
Lung cancer is a complicated disease to treat, so you want your doctor to have as much information as possible about your tumor. Fortunately, medical research into treatments is advancing. Talk to your HCP about your options.
This educational resource was created with support from Daiichi Sankyo and Novocure.
- Lung Cancer Kills an Alarming Number of Women — But There’s Hope ›
- Lung Cancer ›
- Early Screening for Lung Cancer Can Be a Lifesaver ›
- I Never Smoked and Got Lung Cancer ›
- Ask the Expert: Lung Cancer - Risk Factors and Interventions ›
- Lung Cancer 101 ›
- Facts About Lung Cancer Treatments - HealthyWomen ›
- Información acerca de los tratamientos de cáncer pulmonar - HealthyWomen ›
- I’m a Non-Smoker with Stage 4 Lung Cancer - HealthyWomen ›
- Nunca fumé pero tengo cáncer pulmonar de etapa 4 - HealthyWomen ›
- Why Are More Non-Smokers Getting Lung Cancer? - HealthyWomen ›
- ¿Por qué personas que no fuman están desarrollando cáncer pulmonar? - HealthyWomen ›
- Diagnosed with Stage 3 Lung Cancer for Christmas - HealthyWomen ›
- Why Is Lung Cancer Research Underfunded? - HealthyWomen ›
- ¿Por qué la investigación contra el cáncer pulmonar no tiene suficiente financiamiento? - HealthyWomen ›