Each year, almost 20,000 women in the United States are diagnosed with urothelial bladder cancer (UBC). UBC is a disease usually associated with aging because it takes years for the cancer to develop, according to Heather Mannuel, M.D., a medical oncologist at the University of Maryland Greenebaum Comprehensive Cancer Center.
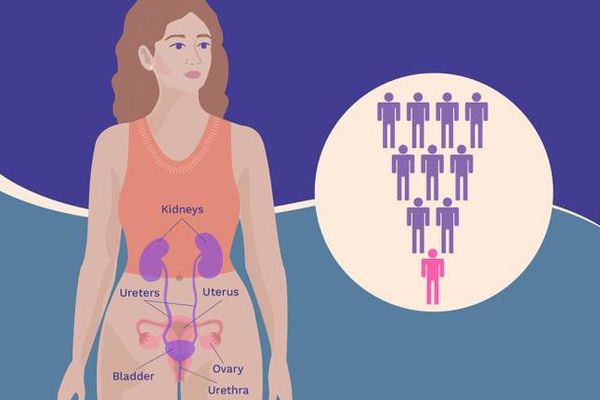
But smoking is a major risk factor for this type of cancer, accounting for between 50% to 65% of new cases. And people who currently smoke are four times more likely to develop UBC than someone who never has.
The relationship between smoking and UBC
Several decades ago, UBC was largely a “man’s disease” because back then, more men smoked than women. But in the mid-1900s, cigarette companies began targeting women. Smoking was promoted as a way to lose weight, look beautiful and be cool. The campaigns were successful and more women started to smoke. Unfortunately, this new habit also brought with it smoking-related diseases like UBC and chronic obstructive pulmonary disease (COPD), so rates of UBC in women climbed.
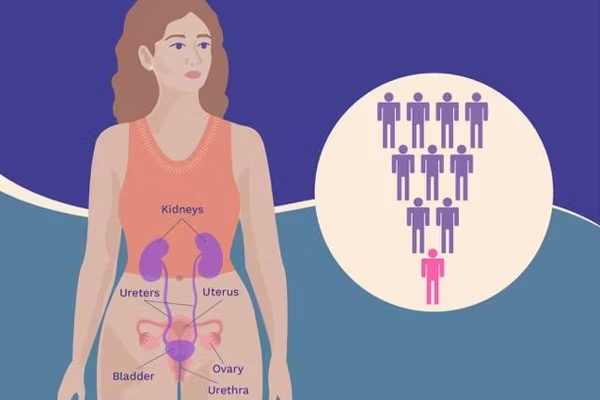
We all understand how smoking can be connected to lung cancer, but its relationship to UBC might not be so clear. As the more than 7,000 chemicals and tars from cigarettes enter your lungs, many break down into toxic byproducts. These byproducts travel through your body and eventually through your kidneys, ending up in your urine. Since urine is constantly sitting in your bladder, the chemicals in the urine start to damage the cells in the bladder wall.
As vaping becomes more popular, there’s concern that this will be another risk factor for UBC. Mannuel said it’s too early to tell because the cancer develops very slowly, over many years. However, researchers are finding concerning biomarkers that are linked to UBC in the urine of people who vape.
Other risk factors for urothelial bladder cancer
Although smoking is a major risk factor for UBC, there are others as well, particularly environmental toxins. Among men, this exposure was often due to chemicals from metals, dyes and paints, especially before workplace regulations were put into place to reduce contact. But with women, it’s frequently those who were exposed to hair dyes. “Hairdressers, people that were hair stylists and colorists for many years, were using dyes that were much harsher,” Mannuel said. “A lot of those women developed bladder cancer down the line.” And if they smoked or they were exposed to cigarette smoke, their risk increased even more.
Other risk factors for bladder cancer include having a bladder malformation or defect, long-term use of urinary catheters, and having frequent urinary tract infections (UTIs).
Who you are, where you live may affect UBC diagnosis and treatment
Women are typically diagnosed later with UBC than men, so while more men have this type of cancer, women end up with cancer that’s further along and more aggressive. It’s then harder to treat. There are several reasons for this, but importantly, it could be related to how women often view urinary problems. Common signs of UBC are the need to urinate often, recurrent bladder infections and blood in your urine.
If these signs happen to men, they tend to seek help because they’re unusual. But many women are used to this happening because UTIs, which cause the same symptoms, are so common. And as women get older, they might chalk the symptoms up to going through menopause before thinking it could be something more serious. So they often delay going to the doctor — believing it’s just part of life as a woman.
Where you live is important too. According to a report published by the Association of Community Cancer Centers, people who live in rural areas or economically depressed areas are less likely to get timely surgery or be treated with chemotherapy. The report also states that people who are female, Black or Hispanic and those who have lower income and education levels are also at an increased risk of being diagnosed with UBC when it’s at a more advanced stage.
It's not too late to reduce your risk for urothelial bladder cancer

iStock.com/Daria Kulkova
We can’t avoid getting older, but we can change some of our behaviors that could reduce the risk of developing UBC. “The number one thing is to stop smoking,” Mannuel said. She acknowledged that it’s not easy to quit, but it’s important.
You can cut your risk of UBC by quitting. If you already have UBC, not smoking improves your recovery and increases survival rates. And it reduces your risk of the cancer coming back.
Here are some tips to help you quit smoking:
- Make your plan. A quit plan helps you pick a date and determine how you will move forward.
- Speak to your doctor about options, such as nicotine replacement therapy (patches, gum, etc.).
- Explore various smoke-free apps, online groups or in-person support groups, including the CDC Quitline.
- Check out the American Cancer Society tips for quitting.
- Ask friends and family for their support.
Mannuel wants women to put themselves and their health first. “When you see something that’s different from your baseline, look into it,” she said. “Don’t shrug it off. Get checked.”
This educational resource was created with support from BD and Merck.
- What Women Need to Know About Urothelial Bladder Cancer ›
- True or False: Urothelial Bladder Cancer ›
- Bladder Cancer and Black Women ›
- Fast Facts: Everything You Need to Know About Urothelial Bladder Cancer ›
- Fast Facts: What You Need to Know About Smoking and Bladder Cancer ›
- How to Quit Smoking - HealthyWomen ›
- Diagnosing Urothelial Bladder Cancer (UBC) - HealthyWomen ›
- The Start and Spread of Urothelial Bladder Cancer - HealthyWomen ›