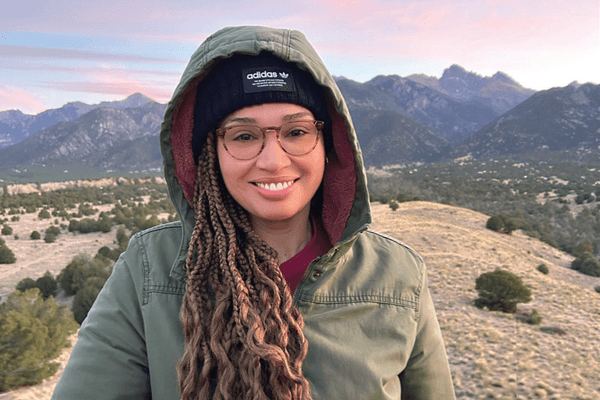
Achea Redd had always been good about getting a yearly mammogram — until the pandemic started. Redd, who is now 41, has been getting mammograms since she was 35, but Covid-19 concerns caused her to postpone in 2020. When the risk of exposure went down, Redd immediately rescheduled. “I didn’t want to wait too long,” she said. “As soon as I could get in and feel safe, I was there.”
Melissa Dominguez, 40, was planning to get her first mammogram in early 2021, but she postponed hers for a different (although also Covid-19-related) reason. She had just gotten her Covid vaccine and was worried it would affect her mammogram results. “I’d heard of women who got their mammogram shortly after the Covid vaccine having false positive results,” she said.
Some experts recommend waiting four to six weeks after getting a Covid vaccine for a mammogram because lymph nodes can become enlarged from the shot. “We, like many organizations, delayed women for six weeks after they received their vaccinations,” said Dr. Debra Somers Copit, a radiologist and former director of breast imaging at Albert Einstein Medical Center.
Dominguez waited, then made the call. As we are likely to be living with Covid vaccines for some time, it’s important that people not put off their preventive healthcare visits but do figure out how to get checked out safely. This includes waiting the necessary time after getting a Covid vaccine for a mammogram but not waiting longer than necessary and taking appropriate safety measures when visiting healthcare facilities.
Delaying breast cancer screenings can be dangerous
Breast cancer screening tools like mammograms are meant to find breast cancer early, before any symptoms (like a lump) develop. Breast cancers found during screenings are generally smaller and are less likely to have spread to other areas of the body, making them easier to treat.
For women at average risk of breast cancer, the American College of Obstetricians and Gynecologists recommends screening every one to two years, starting at age 40.
Unfortunately, breast cancer screenings have declined sharply because of Covid-19. One large study published in the Journal of the American College of Radiology (JACR) found that, in June 2022, all types of mammograms were still at lower levels than they were pre-Covid, with screening mammograms at just 85% of what they had been before the pandemic. .
Not only does the decline in screenings mean delayed or missed breast cancer diagnoses, but it may also widen the inequality gap for people who are already experiencing health disparities. The JACR study found that older women and Asian women were disproportionately affected by delayed screening. Among women of racial and ethnic minority groups with low incomes, breast cancer screening rates went way down when their access to medical services decreased at the beginning of the pandemic.
These disparities highlight the need for equal access to mammograms and other preventive screenings for all women, regardless of factors like race, ethnicity and socioeconomic status.
Breast cancer hits underserved communities hard
Racial and ethnic minorities are affected by breast cancer more than nonminorities. Black women have the highest rate of breast cancer deaths in the United States; Black women are also more likely than other women to be diagnosed with breast cancer at a young age, to be diagnosed at a late stage, and to die from the disease. Black and Hispanic women are also more likely than white women to be diagnosed with aggressive and tough-to-treat triple negative breast cancer.
Women with low incomes and those living in rural areas are also more affected by breast cancer than their more affluent or urban peers. People who live in counties affected by persistent poverty are more likely to die of cancer than those who live in other counties, and rural areas tend to have higher cancer mortality rates than urban and suburban areas. These women may not have access to treatments for breast cancer or to the screenings that help prevent it.
Accessibility is a problem when it comes to getting screened for breast cancer
There are two types of mammograms: 2D (also known as conventional) and 3D. Two pictures are taken of the breast during a 2D mammogram, while a 3D mammogram combines multiple X-rays from many angles to create a three-dimensional picture of the breast. 3D mammography has been shown to be more effective than 2D at detecting breast cancer in women over 65 and may also work better for women with dense breasts.
Women with dense breasts, breasts composed mostly of glandular tissue rather than fat, are at greater risk of breast cancer. In fact, one study found that dense breasts are the number one risk factor for breast cancer, outweighing all other known risk factors.
Redd worries about lack of access in underserved communities to more sophisticated screening tools like the 3D mammogram. “Black women statistically have higher breast density than white women — hence the risk for breast cancer is higher,” Redd said. “Typically, in order to see those types of tumors when they are relatively small you need a 3D mammogram and/or ultrasound. Those tests are more expensive and may not be accessible in urban clinics.”
Dominguez agrees that accessibility is an issue in the Black community, as is faith in the healthcare system. “There is a trust issue because of experiences Black women have had with healthcare providers (HCPs) who were biased or insensitive to their needs,” she said. “We need to do better.”
For women who are already vulnerable to worse outcomes when it comes to breast cancer because of health inequalities, lack of access to mammograms and other screenings can be especially dangerous.
“Screening minorities continues to be an issue for all of us in breast imaging,” Copit said. “I think primary care physicians and OB-GYNs need to reinforce its importance in reducing mortality.”
Overcoming barriers to breast cancer screening
Whether the pandemic has caused you to put off your mammogram or you’re not sure you can afford one, there are steps you can take to make sure you’re keeping up with the preventive breast cancer screenings you need.
If you’re worried about cost, talk to your HCP or visit Freemammograms.org to find free or low-cost mammogram providers in your area.
If you want to schedule a mammogram but aren’t sure where to start, call the National Cancer Institute (800-4-CANCER) or the American College of Radiology (800-227-5463) to find certified mammogram providers near you.
Although Copit understands why some women are tempted to put off mammograms, she believes they get easier over time. Once women get into a routine of having yearly mammograms, she said, they seem to fear it a little less.
This resource was created with support from Hologic.
- Making It Easier to Access Breast Care ›
- Do You Have Dense Breasts? Knowing Your Status Could Make a Difference in Your Breast Cancer Screening ›
- Family History and Breast Cancer Screening ›
- 3 Facts Every Woman Needs to Know About Breast Cancer Screening ›
- Breast Cancer Screening & Testing ›
- Olivia Munn’s Breast Cancer Diagnosis Is a Wake-Up Call for All Women - HealthyWomen ›
- Don't Postpone These Types of Preventive Care - HealthyWomen ›