If you suffer from atopic dermatitis (AD), you’re not alone. It’s the most common form of eczema, affecting nearly 16.5 million Americans. Women experience AD more than men, and women between the ages of 15 and 49 are more likely to experience more severe symptoms.
Although eczema has no cure, multiple treatment options are available. Learn more about the AD therapies currently on the market, how they work and what their long-term effects are, and talk to your healthcare provider (HCP) about what might be the best option for you.
Over-the-counter therapies
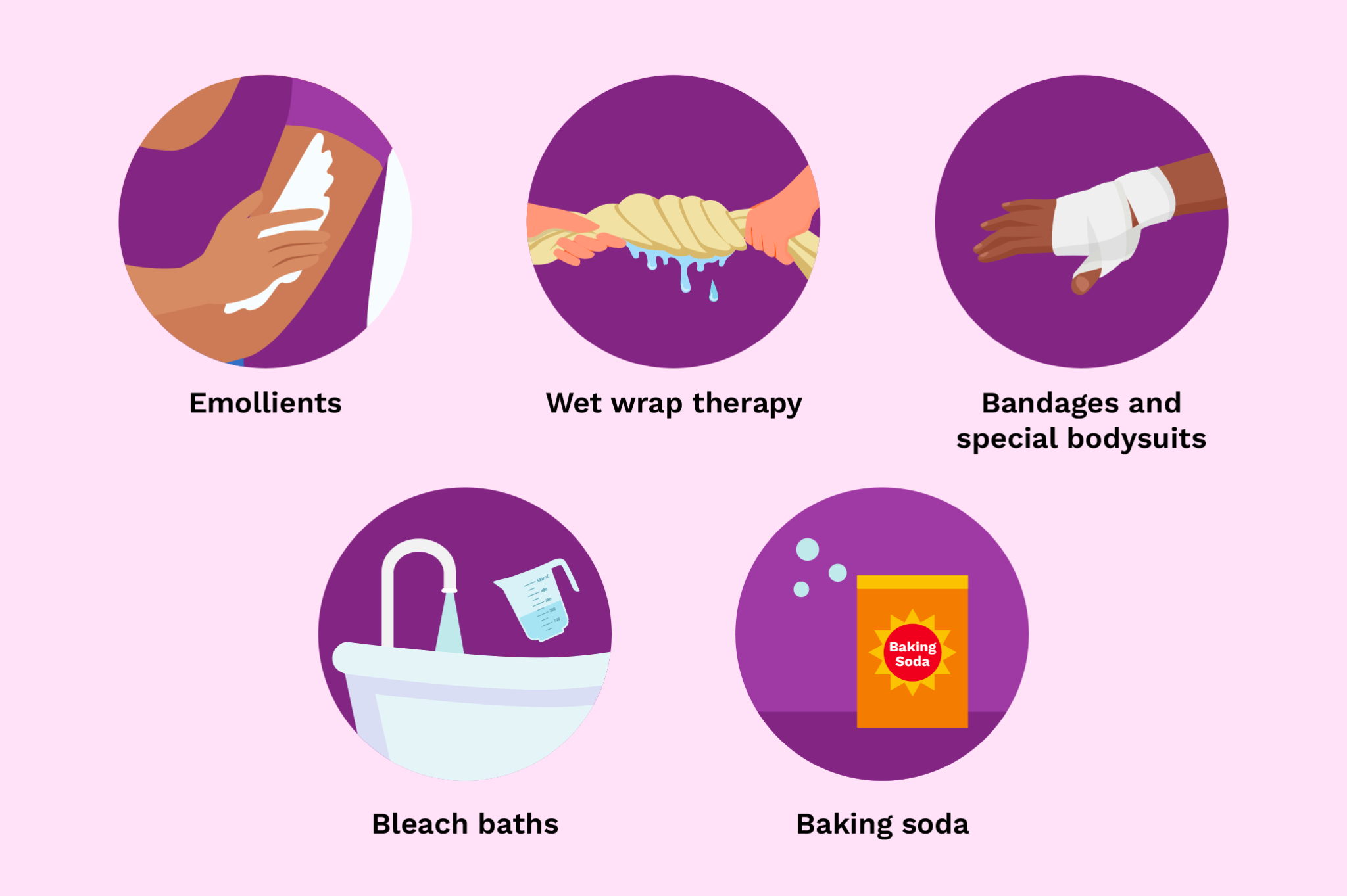
Your HCP might suggest a combination of prescription and over-the-counter treatments to help manage AD. Here are a few of the most common ones you can obtain without a prescription.
- Emollients like moisturizers, creams, lotions and ointments have long been used to manage and control eczema by maintaining the moisture level of the skin. These are critical to help all individuals manage AD.
- Wet wrap therapy can rehydrate the skin and help your topical medications work more effectively. To perform wet wrap therapy, individuals should take lukewarm baths, moisturize, apply topical medication (either OTC or prescription), and then use wet clothing or gauze to cover the skin. A dry layer should be placed on top of the wet layer after that.
- Bandages and special bodysuits have been designed for standalone use or with wet wrap therapy, including some that are already medicated. The bodysuits look similar to pajamas, and your HCP might refer to them as wet pajamas or dry pajamas.
- Bleach baths may reduce the amount of bacteria on the skin that can lead to infection, as well as decrease itching and inflammation.
- Baking soda added to your bathwater or applied directly to the skin as a paste can also decrease itching.
Prescription therapies
The order that these prescription therapies are offered can depend on the areas affected by AD and the preferences of patients and their HCPs.
Topicals
The most common topical treatments for AD fall into five general categories.
- Topical steroids — both prescription and over-the-counter — have been used for decades to treat AD in adults and children. They help reduce inflammation and itching and are usually the first line of treatment for mild to moderate AD.
- Topical calcineurin inhibitors (TCIs), such as Protopic, Elidel and generic equivalents, are nonsteroidal ointments and creams that work by suppressing immune system cells that would trigger AD symptoms. They can be used anywhere on the body and generally take about a week to start working.
- Topical phosphodiesterase 4 (PDE4) inhibitors, such as Eucrisa, are also nonsteroidal and work by blocking the PDE4 enzyme that can trigger the inflammation that leads to AD. A topical PDE4 inhibitor ointment is available by prescription for AD treatment.
- Prescription barrier creams mimic the outer layer of the skin, reducing water loss and possibly decreasing flares. They’re nonsteroidal and can be used anywhere on the body.
- Topical Janus kinase (JAK) inhibitors, such as Opzelura, block the Janus kinase enzymes that can lead to inflammation that triggers AD. The topical JAK inhibitor for AD is safe for use for patients age 12 and over, but only for two weeks or less. This medication should only be used if other therapies have not worked.
Injectables
These medications can be delivered through the skin or through veins. As “biologics,” they use human DNA to treat AD at the immune system level. Biologics are usually prescribed only if other treatments haven’t proven effective or patients are unable to use other treatments. HCPs generally reserve injectables for patients with moderate to severe AD.
- Dupilumab, known as Dupixent, is safe for patients over 6 and requires no lab monitoring. It can also treat asthma, nasal polyps and chronic rhinosinusitis. Dupilumab can increase the risk of getting conjunctivitis (pink eye).
- Tralokinumab, known as Adbry, is approved only for adults with moderate to severe AD.
Oral medications
Multiple categories of pills can be used to treat AD. The pills work to control or suppress the immune system to minimize AD symptoms and are often prescribed for moderate to severe AD.
- Traditional systemic medications, which include cyclosporine and methotrexate as well as some other therapies, are designed to only be used for short periods of time to control moderate to severe AD before patients switch to topical medications. The pills in this category are considered “off-label,” meaning they are not approved by the FDA to treat AD.
- Two oral JAK inhibitors, CIBINQO and Rinvoq, are on the market for those who can’t use biologics. One is available for adults only and the other can be used by those 12 and over. These are used very sparingly and often reserved for people with severe AD who have not had success with other treatments.
- Steroids can be prescribed for the most severe AD cases, but should only be used for short-term treatment (less than a month). They can manage inflammation, but AD symptoms can return and be even worse after discontinuing the medication.
Phototherapy
Phototherapy consists of treatment by a HCP with ultraviolet (UV) light several times a week. It’s often called light therapy, and it helps minimize itch and inflammation. This form of treatment might be recommended for AD all over the body or AD that’s located in one or two areas of the body. It’s usually prescribed if topicals haven’t been working.
This resource was created with support from AbbVie, Regeneron and Sanofi.
- Eczema Cost Me My Self-Esteem. Now, I'm on the Path to Getting It ... ›
- What Is Step Therapy? - HealthyWomen ›
- Clinically Speaking: Questions to Ask Your Healthcare Provider ... ›
- Atopic Dermatitis Across Your Body - HealthyWomen ›
- Living With Atopic Dermatitis (AD) - HealthyWomen ›
- Ask the Expert: Atopic Dermatitis - HealthyWomen ›
- How Atopic Dermatitis Changes as You Age - HealthyWomen ›