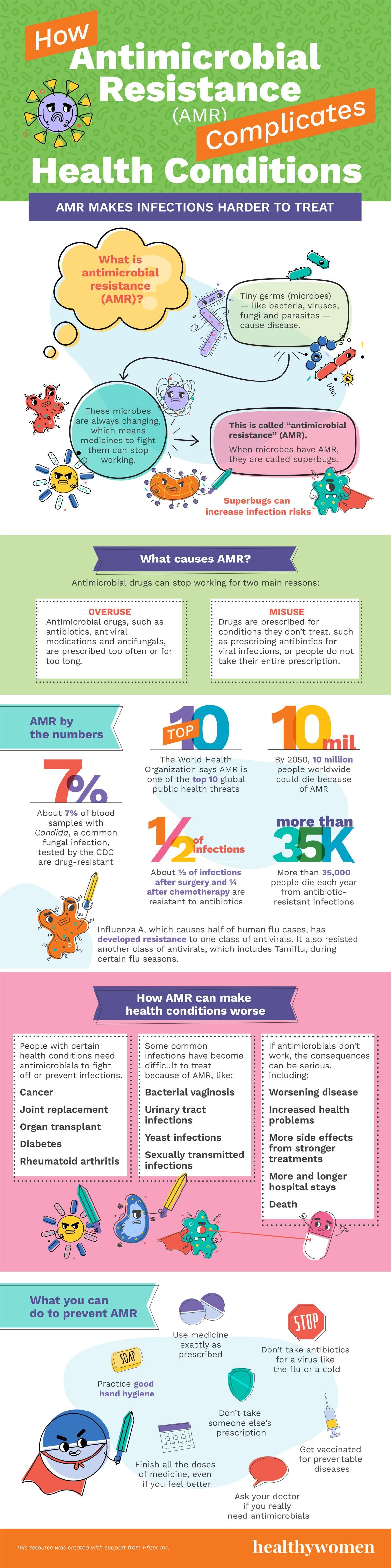
What is antimicrobial resistance (AMR)?
Tiny germs (microbes) — like bacteria, viruses, fungi and parasites — cause disease.
These microbes are always changing, which means medicines to fight them can stop working.
This is called “antimicrobial resistance” (AMR).
When microbes have AMR, they are called superbugs.
AMR makes infections harder to treat.
What causes AMR?
Antimicrobial drugs can stop working for two main reasons:
- Overuse: Antimicrobial drugs, such as antibiotics, antiviral medications and antifungals, are prescribed too often or for too long.
- Misuse: Drugs are prescribed for conditions they don’t treat, such as prescribing antibiotics for viral infections, or people do not take their entire prescription.
AMR by the numbers
- The World Health Organization says AMR is one of the top 10 global public health threats
- By 2050, 10 million people worldwide could die because of AMR
- More than 35,000 people die each year from antibiotic-resistant infections
- About 7% of blood samples with Candida, a common fungal infection, tested by the CDC are drug-resistant
- About ½ of infections after surgery and ¼ after chemotherapy are resistant to antibiotics.
Influenza A, which causes half of human flu cases, has developed resistance to one class of antivirals. It also resisted another class of antivirals, which includes Tamiflu, during certain flu seasons.
How AMR can make health conditions worse
People with certain health conditions need antimicrobials to fight off or prevent infections.
- Cancer
- Joint replacement
- Organ transplant
- Diabetes
- Rheumatoid arthritis
Some common infections have become difficult to treat because of AMR, like:
- Bacterial vaginosis
- Urinary tract infections
- Yeast infections
- Sexually transmitted infections
If antimicrobials don’t work, the consequences can be serious, including:
- Worsening disease
- Increased chronic health problems
- Infection not having been adequately treated
- More side effects from stronger medications
- More and longer hospital stays
- Death
What you can do to prevent AMR
- Use medicine exactly as prescribed
- Finish all the doses of medicine, even if you feel better
- Don’t take antibiotics for a virus like the flu or a cold
- Don’t take someone else’s prescription
- Ask your doctor if you really need antimicrobials
- Practice good hand hygiene
- Get vaccinated for preventable diseases
This resource was created with support from Pfizer Inc.
- The Global Threat of Superbugs - HealthyWomen ›
- I Contracted a Superbug That's a Top Public Health Threat — And ... ›
- Why Antimicrobial Resistance Is a Threat We Need to Take ... ›
- Clinically Speaking: Important Questions to Ask About Antimicrobial ... ›
- You, Too, Can Fight AMR! - HealthyWomen ›
- Q&A: How Fighting Superbugs Could Help Prevent the Next Pandemic - HealthyWomen ›
- AMR 101 With Dr. Uzma Syed - HealthyWomen ›
- How Superbugs Put Cancer Patients at Risk - HealthyWomen ›
- Antimicrobial Resistance and Women - HealthyWomen ›