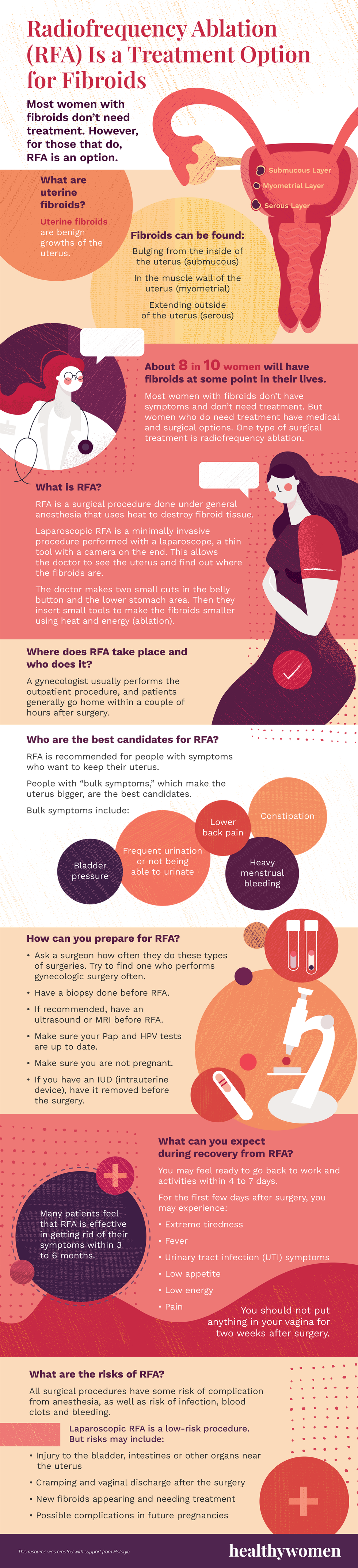
What are uterine fibroids?
Uterine fibroids are benign growths of the uterus.
Fibroids can be found:
- Bulging from the inside of the uterus (submucous)
- In the muscle wall of the uterus (myometrial)
- Extending outside of the uterus (serous)
About 8 in 10 women will have fibroids at some point in their lives.
Most women with fibroids don’t have symptoms and don’t need treatment. But women who do need treatment have medical and surgical options. One type of surgical treatment is radiofrequency ablation.
What is RFA?
RFA is a surgical procedure done under general anesthesia that uses heat to destroy fibroid tissue.
Laparoscopic RFA is a minimally invasive procedure performed with a laparoscope, a thin tool with a camera on the end. This allows the doctor to see the uterus and find out where the fibroids are.
The doctor makes two small cuts in the belly button and the lower stomach area. Then they insert small tools to make the fibroids smaller using heat and energy (ablation).
Where does RFA take place and who does it?
A gynecologist usually performs the outpatient procedure, and patients generally go home within a couple of hours after surgery.
Who are the best candidates for RFA?
RFA is recommended for people with symptoms who want to keep their uterus.
People with “bulk symptoms,” which make the uterus bigger, are the best candidates.
Bulk symptoms include:
- Bladder pressure
- Frequent urination or not being able to urinate
- Lower back pain
- Constipation
- Heavy menstrual bleeding
How can you prepare for RFA?
- Ask a surgeon how often they do these types of surgeries. Try to find one who performs gynecologic surgery often.
- Have a biopsy done before RFA.
- If recommended, have an ultrasound or MRI before RFA.
- Make sure your Pap and HPV tests are up to date.
- Make sure you are not pregnant.
- If you have an IUD (intrauterine device), have it removed before the surgery.
What can you expect during recovery from RFA?
You may feel ready to go back to work and activities within 4 to 7 days.
For the first few days after surgery, you may experience:
- Extreme tiredness
- Fever
- Urinary tract infection (UTI) symptoms
- Low appetite
- Low energy
- Pain
You should not put anything in your vagina for two weeks after surgery.
Many patients feel that RFA is effective in getting rid of their symptoms within 3 to 6 months.
What are the risks of RFA?
All surgical procedures have some risk of complication from anesthesia, as well as risk of infection, blood clots and bleeding.
Laparoscopic RFA is a low-risk procedure. But risks may include:
- Injury to the bladder, intestines or other organs near the uterus
- Cramping and vaginal discharge after the surgery
- New fibroids appearing and needing treatment
- Possible complications in future pregnancies
This resource was created with support from Hologic.
- Fibroids ›
- Heavy Menstrual Bleeding: Symptoms and Treatment ›
- Clinically Speaking: What Are My Options Following a Uterine Fibroid Diagnosis? ›
- What Are the Surgical Treatments for Fibroids? - HealthyWomen ›
- Surgical Options for Fibroids - HealthyWomen ›