By Sarah Lynch, Binghamton University, State University of New York and Danielle Mayer, Thomas Jefferson University
The new year has brought the deadliest weeks of the U.S. COVID-19 epidemic thus far, with thousands of deaths every day. It's been several weeks since the U.S. Food and Drug Administration issued the first of two emergency use authorizations for COVID-19 vaccines, but getting one isn't easy.
There are no available appointments to get a vaccine in many communities. Wait times at California's Dodger Stadium, the nation's largest distribution site, reached five hours earlier this month. At the current rate, it could take until 2022 for all adult Americans to be vaccinated, according to some estimates.
The Biden administration is trying to change that. The national strategy President Biden rolled out in his first week in office includes a target of injecting 100 million vaccines during his first 100 days as president and strengthening distribution to high-risk communities.
A key component of the president's five-step vaccine plan, he said, is to “fully activate the pharmacies across the country." This will greatly expand the number of providers to administer vaccines – and expand the role of pharmacists in the pandemic in the weeks and months ahead.
As pharmacists who work in both rural and urban settings, we are among those who are preparing to meet this challenge.
Challenges with handling and distribution
With the slow rollout, community pharmacies are being brought on board much sooner than anticipated. They've been an underutilized resource: U.S. pharmacies have experience storing and administering many types of vaccines. In 2018, they gave about one-third of all flu shots, up from 18% in 2012. They are now preparing to handle the new Pfizer-BioNTech and Moderna COVID-19 vaccines.
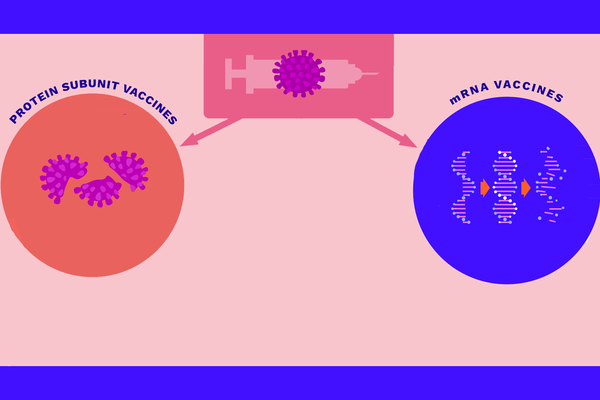
These messenger RNA (mRNA) vaccines have a new, but not unknown, mechanism. The Moderna vaccine can be kept in a traditional freezer, but the Pfizer vaccine requires ultra-cold storage at -112 to -76 F before being thawed and administered. Health systems and federal partner pharmacies equipped with these specialized freezers are key hubs for distribution.
It's not just the vaccine that needs to be protected. Pharmacies are stockpiling personal protective equipment to keep staff safe. They have also established safety protocols for patients – social distancing, disinfection and observation for 15 to 30 minutes after vaccination.
There are also administrative requirements, issuing immunization cards to those who have been immunized and reporting the number of administered doses to state and federal officials.
Pharmacies are registering with the searchable Vaccine Finder website – where people will be able to search for participating pharmacies. The vaccine is free: Insurance companies will be billed an administration fee, though a national relief fund covers that cost for the uninsured.
Under a U.S. Department of Health and Human Services mandate, pharmacists and pharmacist interns who have completed a minimum of 20 hours of accredited training are authorized to administer COVID-19 vaccines.
Sharing information
While health departments and local officials are working to share information, many people are calling their local pharmacies with questions. Because the vaccine was produced, tested and approved in record time, some are questioning its safety. It was produced quickly because government funding fast-tracked various phases of development, allowing them to be conducted simultaneously rather than sequentially. Thousands of volunteers signed up for clinical trials, speeding the process, and emergency FDA approval allowed for rollout while some phase 3 studies are completed.
People are also concerned about contracting coronavirus from the vaccine, which is impossible. Neither mRNA vaccine contains live virus; they simply teach the body to recognize the unique spike protein on the outside of the COVID-19 virus to create a faster immune response to the invader if exposed. Two doses must be spaced 21 to 28 days apart, and it takes another few weeks after the second dose to reach full immunity.
Some who have called us are worried about possible side effects. The most commonly reported aftereffect is pain and swelling at the injection site; some individuals have also reported chills, fever, headache or fatigue. While this may be uncomfortable, it's not alarming: These are all signs that the immune system is doing its job.
We have also helped explain to people why all are monitored after their shot. A few people have had serious allergic reactions – anaphylactic shock, which is why there is an established observation period after the vaccine that is longer for anyone with a history of allergies. Pharmacists are trained to respond to these rare reactions should they occur.
There have also been reports of individuals who have died within days or weeks of receiving the vaccine. Researchers are investigating these rare events, but so far, there is no evidence that the vaccine is responsible. Unrelated or “incidental" illness seems to be the culprit, which is unsurprising given the demographics – many of those vaccinated in the early rollout are elderly people who are in frail health.
Vaccines have the power to bring this pandemic under control. They could possibly even end it, but only after some 70% of humanity is inoculated. Almost 90% of Americans live within five miles of a local pharmacy where, starting in February, many will be able to get vaccinated against this virus.
[Research into coronavirus and other news from science Subscribe to The Conversation's new science newsletter.]![]()
Sarah Lynch, Director of Skills Education and Clinical Assistant Professor of Pharmacy Practice, Binghamton University, State University of New York and Danielle Mayer, Assistant Professor, Department of Pharmacy Practice, Jefferson College of Pharmacy, Thomas Jefferson University
This article is republished from The Conversation under a Creative Commons license. Read the original article.