October 1, 2025, is World Urticaria Day.
Urticaria is the medical word for hives — itchy red welts that appear on your skin. Acute urticaria happens in response to an allergy or some other source you can identify, like sun exposure. The welts usually go away with time or treatment. But chronic spontaneous urticaria, or CSU, are hives that occur suddenly, last for more than six weeks and, unlike acute urticaria, have no known cause.
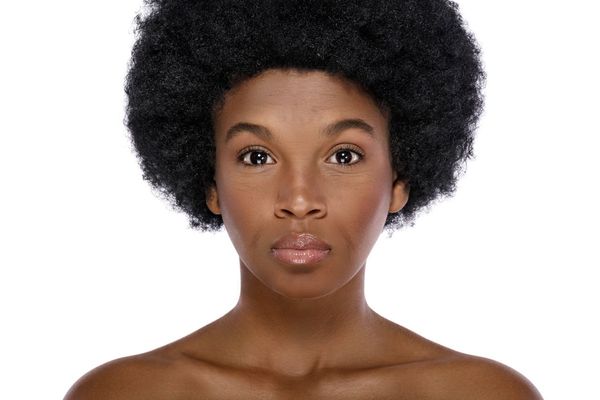
About 1% of people around the world get CSU. Most get it when they’re in their 20s to 40s, although you can get it at any age — even childhood. Women are twice as likely to get CSU than men, and Black and non-white people get it more often than white people. Lower socioeconomic status can also increase your chances for CSU.
Having hives may seem harmless, but the constant, long-term itching from the welts can have a strong impact on your quality of life. And, if you scratch them, they could become infected.
CSU Symptoms
CSU welts may look like bug bites, but there are differences. The hives:
- Appear anywhere on the body, especially along the waist, under the arm and in the groin
- Change shapes
- Disappear and reappear
- Move to different locations
- Look red or skin color
- Turn white or disappear when you press on them
If you’ve been scratching, you might see scratch marks and blood as well.
CSU Causes
Unlike acute hives, the cause of chronic hives is unknown. Researchers believe that half the time, CSU is caused by an autoimmune problem, and your body is sending out histamine, which is a chemical your body releases to fight allergies. Almost 1 in 10 people with CSU have an autoimmune disease, like rheumatoid arthritis or Type 1 diabetes.
If you have CSU, you might notice that some situations can make it worse, like when you’re stressed or have an infection, or when you’re cold.
Diagnosing CSU
Your healthcare provider (HCP) will determine if you have acute urticaria or CSU. They’ll ask for a detailed medical history, looking for allergies or anything that could explain the hives. A physical exam is next, looking at the hives and where they are.
Blood tests don’t diagnose CSU, but they can rule out other causes and even check for autoimmune diseases if your HCP suspects this might be the case.
Treating CSU
Your HCP might refer you to an allergist, immunologist or dermatologist. The first treatment will likely be antihistamines (allergy medications). However, antihistamines aren’t effective for most people with CSU. If they don’t work, omalizumab, which is also used for asthma, might be the next option, but many people don’t have success with omalizumab either. A third option is cyclosporine, which suppresses the immune system.
Researchers are also looking for alternative medications for people with CSU. In 2025, the Food and Drug Administration approved a biologic medicine called dupilumab, which controls inflammation by blocking the immune system, and there are other biologics that are still undergoing clinical trials. These medications could be added to other treatments or help people who have not been able to control their CSU with existing treatments.
Support for people living with CSU
If you have CSU, you’re not alone. There are organizations dedicated to helping people with CSU, such as We CU and the Chronic Urticaria Patients Support Group Association. You can also join the Chronic Urticaria Registry. You’d be helping with a global research project looking at what causes CSU, as well as its diagnosis and treatment.
Resources
American College of Asthma, Allergy, and Immunology
Asthma and Allergy Foundation of America
This educational resource was created with support from Sanofi, a HealthyWomen Corporate Advisory Council member.