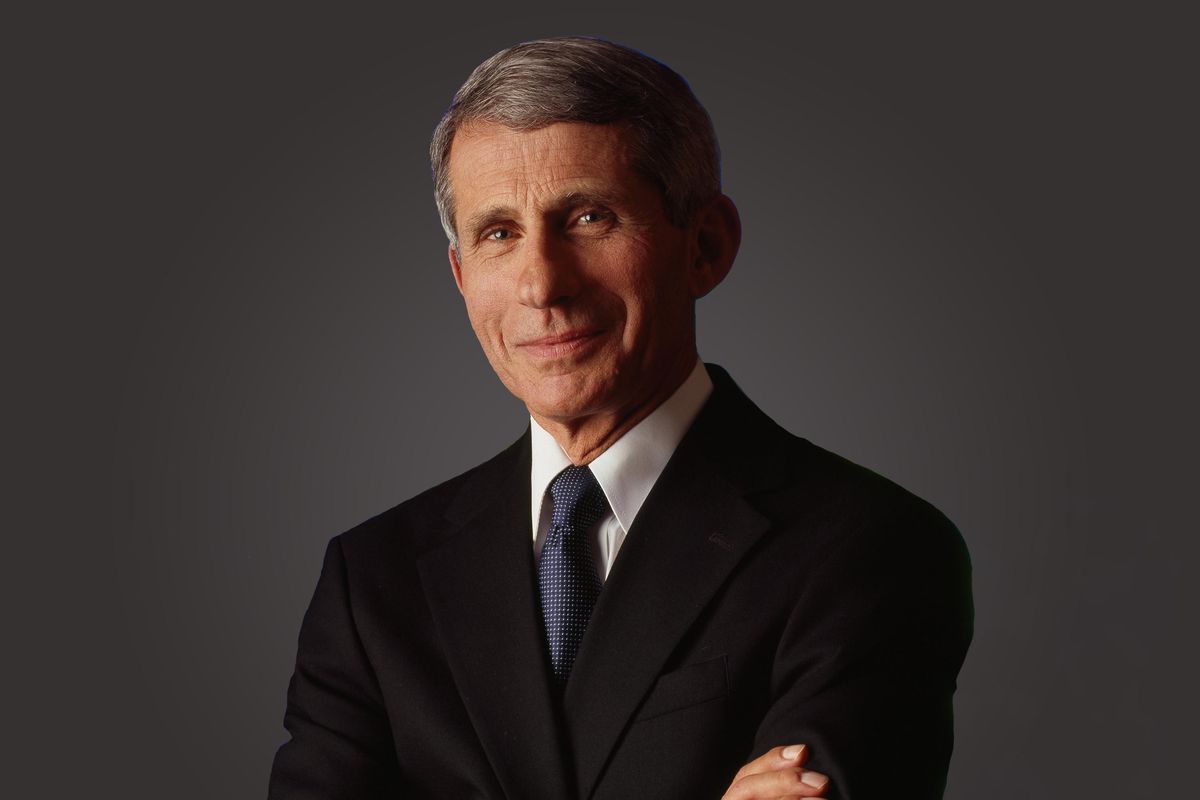
HealthyWomen's editor-in-chief, Jaimie Seaton, recently spoke with Dr. Anthony Fauci. As the director of the National Institute of Allergy and Infectious Diseases (NIAID), chief medical advisor to President Biden, and a practicing physician, he's an extraordinarily busy man. So, we were honored when he agreed to give us 15 minutes from 5:00 to 5:15 to shed some light on all things COVID-19. We talked about everything from the new Johnson & Johnson COVID-19 vaccine to the importance of masking.
The transcript has been lightly edited for clarity and length.
HealthyWomen: Are people able to choose which vaccine they get? If so, what would make Johnson & Johnson worth choosing, given the fear of the lower efficacy rate?
Dr. Fauci: Well, first of all, I think you need to separate the Moderna and Pfizer from the J&J. If you were to say, "Can people choose between, let's say Moderna or Pfizer," it's very difficult to do because you usually will go to a place that has vaccine available, and whatever they happen to have between the two of them, then that's the one you'll take. But in general, since they're so equivalent — they're almost identical — there really is no need for a choice.
But with the J&J, that's going to be an issue that I think is going to be decided when you get all of the data that's examined by the FDA and the Advisory Committee on Immunization Practices.
[When the data is fully scrutinized], it may be that the J&J vaccine is more preferable for this particular demographic group or for this particular situation. We don't know that. If, in fact, it doesn't make any difference one way or another, then people could have their choice. They may say, "You know, I'm balancing the fact that it's a one shot vaccine, which I know can be very effective in preventing serious illness, hospitalizations and death, and that's really what I'm interested in. I don't want to get seriously ill." Another person will say, "Well you know, I'd rather get the 94 to 95% effective vaccine even if it's two shots because I don't even want to get mild to moderate illness." It depends on people's preference, and they're going to be making their choice on that.
HealthyWomen: What do you say to those who want to wait to get the vaccine because of the new strains? Can you talk a little bit about the mutations and how they occur, when a virus spreads, and how it replicates?
Dr. Fauci: First of all, RNA viruses have a strong tendency to mutate. Any RNA virus, but particularly this one, will mutate; the more you replicate, the more likely you're going to mutate. So the best possible thing that we can do to prevent or slow down the process of mutation is to vaccinate as many people as we possibly can as quickly as we possibly can.
It doesn't make any sense to wait to get vaccinated because you want to wait until we match a booster or a new vaccine to match the mutant because we know already from the studies of J&J in South Africa, as well as the studies that the UK did in South Africa with another candidate, that you can get good protection against serious disease, even against the mutants. So it doesn't make any sense to not get vaccinated because you're waiting for a better vaccine. It makes much more sense to protect yourself against all of it because we know that the vaccines that are currently available work quite well to prevent serious disease, namely the J&J vaccine particularly.
HealthyWomen: So for those who've already been vaccinated with the Pfizer and the Moderna vaccine, do we know if they are protected against the South African and other variants?
Dr. Fauci: We don't know. It is entirely conceivable and likely that you get some protection against the South African variant with the Moderna and the Pfizer. We don't know because we haven't tested it yet. But if you look at the fact that the J&J vaccine protected against serious disease with the mutants, it is likely that the Moderna and the Pfizer vaccine, even though we have not formally tested it yet against the new mutant, will perform at least as well as the J&J did.
HealthyWomen: After getting vaccinated, I understand that it's still possible to get COVID-19 within a 14-day window. Can you still get sick from the virus beyond the 14-day window, and can you still spread the virus if you've been vaccinated?
Dr. Fauci: Well first of all it depends on what vaccine you're talking about. Are we still talking about J&J, or are we talking about Moderna and Pfizer?
HealthyWomen: Let's start with Moderna and Pfizer.
Dr. Fauci: With Moderna and Pfizer, you have a 94 to 95% chance of protection against clinically recognizable disease, starting when you are about seven to 14 days following the second dose. That's a 94 to 95% chance. Does it protect against infection? We don't know the answer to that yet. We will be able to determine that in studies that will be ongoing where you determine the concentration or the titer of virus in the nose of people who have asymptomatic infections who were vaccinated, compared to those who have asymptomatic infection who were not vaccinated. So the answer is, we do not know if the vaccine protects you against infection.
So, it is conceivable that you could spread the virus when you have no symptoms at all because the vaccine protects you against symptomatic disease, but it doesn't protect you necessarily against infection. We do know that it protects you 94 to 95% against symptomatic disease, but at this point it is uncertain whether it protects you against infection.
HealthyWomen: What about the J&J vaccine?
Dr. Fauci: Again, we know less about that right now. Because we do know that the J&J vaccine, against the United States strains, is 72% effective. However, it's quite effective, 88%, against severe disease from the mutant. Also, similar to the Moderna and the Pfizer, we still don't know yet whether it protects against true infection.
HealthyWomen: With different populations being vaccinated at different rates, how do we interact? When can people start changing their behavior after they've been vaccinated in terms of wearing masks, social distancing and interacting with family members who haven't been vaccinated?
Dr. Fauci: If you are just a vaccinated person in a vacuum and the country has not gotten vaccinated — in other words, we don't have herd immunity yet — you really have to be careful about abandoning public health measures. So that's the reason why we tell vaccinated people, particularly when they're interacting with unvaccinated people, that they really should wear a mask. Because if you are infected and you don't know it, since you've been protected against clinical infection but not actually infection, you could inadvertently infect someone else.
Also, the average is 94 to 95% effective. You don't know 100% whether you're 95% effective. We know as a group, the groups who are vaccinated are 94 to 95% protected. But you're not a hundred percent certain that you are. You might be a little bit less. So it pays, until the level of virus in the community goes very, very low, approaching what we call herd immunity, it makes sense that you should not abandon all public health measures such as wearing of masks.
HealthyWomen: When do you expect the U.S. will reach herd immunity? Or are you able to venture any comment on that?
Dr. Fauci: I can make a comment, but it is just an estimate. People have to understand that this is not definitive. It's just an estimate. And my estimate based on a number of things that you can extrapolate from, is somewhere around when 70 to 85% of the population is vaccinated.
HealthyWomen: Do you have any timeline for that, or is it still too difficult to determine with the problems with the distribution?
Dr Fauci: It depends on how much vaccine hesitancy we get. If we can get over the problem and the issue of vaccine hesitancy, we could reach that sometime by the end of the summer so that by the time we get to the early fall, we could get herd immunity. But that's not a guarantee. That's going to depend very much on whether we can overcome some degree of vaccine hesitancy, which we know exists.
HealthyWomen: Communities of color, as you know, have high infection rates and low vaccination rates, and I wondered what's being done to strengthen trust in the vaccine and close that gap with vaccination rates in communities of color?
Dr. Fauci: Well there's an extraordinary amount of effort. I myself spend a portion of every day reaching out to minority communities to explain to them why it's important for them to get vaccinated to protect their own health, the health of their family, and the health of their community. We also have a task force on equity, which also is very much involved, to see if we can get the minority communities vaccinated. So a lot of effort is being put in by reaching out to brown and Black people in the minority community to try and get them to get involved, not only in joining in the clinical trials, but also, once any vaccine is approved, to actually go out and get vaccinated.
HealthyWomen: There's been a lot in the news lately about double masking. Can you talk a bit about that?
Dr. Fauci: The most important thing is to wear a mask. That is what the CDC recommends. I was asked, You know some people feel, if you're looking at a physical barrier and one mask is good, maybe two masks might be better — one for maybe better protection, and two, you put one mask over the other, you often get a much better fit. And what I said in response to that was: There's nothing wrong with doing two masks; we don't have the scientific data yet to indicate that two masks are better than one mask, even though common sense would tell you that if it's a physical barrier, two physical barriers are better than one. But we don't have the scientific data and the study to confirm that. So my feeling and my position would be: If someone feels that they want to wear two masks, that's fine. There's nothing wrong with that. It might be better, but we don't know that yet.
HealthyWomen: Is there something that the public doesn't know about the pandemic or the vaccine that they should?
Dr. Fauci: Well that's a tough question. I mean (laughs) I'm sure there's a lot of things.
HealthyWomen: I know, but if you had to pick one. Because I know there is a lot of false information out there and there's a lot of good information as well. But is there something that you feel like is not getting enough attention or that the public needs to know?
Dr. Fauci: Well I think what the public doesn't fully appreciate is that the data indicate clearly that masks and other types of nonpharmacologic intervention really do work, and the data are strong in showing that they work. Very often people say, Well some people say masks work; some people say they don't. That merely causes confusion. Wearing of masks does work.
Anyway I gotta run, it's 5:20.