September 25, 2024, is World Dense Breast Day.
Mammograms? Nobody likes to have their breasts squished like a pancake. But now there’s a new reason to make sure you schedule one.
As of September 2024, the Food and Drug Administration (FDA) is requiring that all mammogram reports include information about your breast density. This is a big step in the right direction for women’s healthcare. In the United States, 50% of women over the age of 40 have dense breasts, making it difficult to detect breast cancer before it spreads.
This new ruling keeps women informed, empowering them to discuss additional testing options with their healthcare providers.
Here’s everything you need to know about dense breasts, and what to do if your mammogram report says you have them.
What are dense breasts?
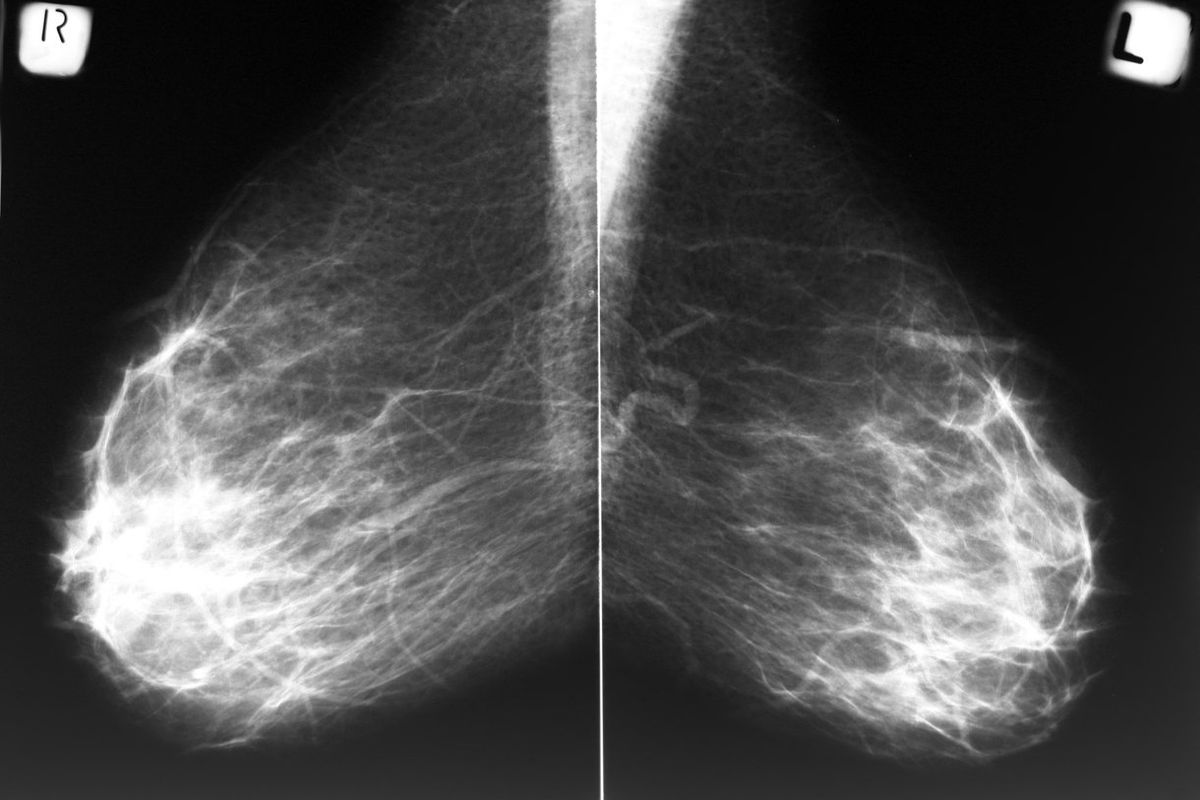
Breast density is the measurement of fibrous and glandular tissue in your breast compared to fatty tissue. The more fibrous and glandular tissue you have, the more difficult it will be to detect cancer on a mammogram.
The amount of density in your breast can be inherited. Women who have a low body mass index or take menopausal hormone therapy may have a higher breast density. However, as you age, your breasts may become less dense. Having children may also reduce your breast density.
How do you know if you have dense breasts?
Whether you have dense breasts or not has nothing to do with how big or how firm your breasts are. The only way to know if you have dense breasts is to have imaging, such as a mammogram. After your mammogram, a radiologist will look for abnormalities in your breasts and determine which category of density your breasts fall into.
The four categories of breast density are:
- Almost entirely fatty: Easy to detect masses or other abnormalities.
- Scattered areas of fibroglandular density: Mammogram shows some white areas.
- Heterogeneously dense: More of the breast is dense, meaning there are more white areas, making it harder to see small masses.
- Extremely dense: The breasts are so dense, it’s difficult to see masses.
If your breasts fall into the first or second category, your breasts are not considered dense.
If your breasts are heterogeneously dense or extremely dense, they are considered dense.
What will your mammogram report say?
Thanks to the recent ruling by the FDA, your mammogram report will clearly state “dense” or “not dense.”
If you don’t have dense breasts, your report will say:
“Breast tissue can be either dense or not dense. Dense tissue makes it harder to find breast cancer on a mammogram and also raises the risk of developing breast cancer. Your breast tissue is not dense. Talk to your healthcare provider about breast density, risks for breast cancer, and your individual situation.”
If you have dense breasts, your report will say:
“Breast tissue can be either dense or not dense. Dense tissue makes it harder to find breast cancer on a mammogram and also raises the risk of developing breast cancer. Your breast tissue is dense. In some people with dense tissue, other imaging tests in addition to a mammogram may help find cancers. Talk to your healthcare provider about breast density, risks for breast cancer, and your individual situation.”
The mammogram report sent to your doctor will include an assessment of your breast density using one of the four categories described above.
Does having dense breasts put me at a higher risk for cancer?
The short answer is yes. Women and people assigned female at birth who have dense breasts have a higher risk of breast cancer, though it’s unclear why.
Black women are more likely to have extremely dense breasts than white women, putting them at greater risk of having undetected breast cancer at early stages. Studies show that Black women are often diagnosed with breast cancer at a later stage and have a higher mortality rate.
In addition, dense breasts make it difficult to see abnormal changes. Glandular tissue and cancerous masses both appear white on a mammogram, making it hard to tell them apart. Unlike dense breasts, fatty tissue appears as mostly black on a mammogram, making it easier to see tumors.
What tests are available for women with dense breasts?
If you have dense breasts, you should still get a mammogram. Then talk to your doctor about additional testing.
Additional tests for women with dense breasts include:
- 3D mammography: Unlike 2D mammography, this imaging moves around the breast in an arc, allowing the radiologist to see the breast tissue more clearly.
- Breast ultrasound: Using a doppler, this painless test uses sound waves to take computer pictures of your breasts. Ultrasounds can get a more detailed look at a suspicious spot that may have been detected on a mammogram.
- Magnetic Resonance Imaging (MRI): This test is used along with a mammogram for women who are at a high risk of breast cancer. However, MRIs are not recommended for women with an average risk of breast cancer because they can have false positives. This can lead to women getting further testing and biopsies that aren’t necessary. To find out if you are at high risk for breast cancer, ask your doctor about the Breast Cancer Risk Assessment Tool.
This educational resource was created with support from Daiichi Sankyo.
- How to Tell if You Have Dense Breasts ›
- My Cancer Was Missed Because of Dense Breast Tissue ›
- Dense Breasts ›
- Do You Have Dense Breasts? Knowing Your Status Could Make a Difference in Your Breast Cancer Screening ›