The American Cancer Society estimates that over 20,000 women in the United States will be diagnosed with bladder cancer in 2024. While bladder cancer happens less often in women than in men, women are more likely to have advanced stages and lower survival rates. Bladder cancer is also more likely to happen in your later years — about 9 out of 10 people are over the age of 55.
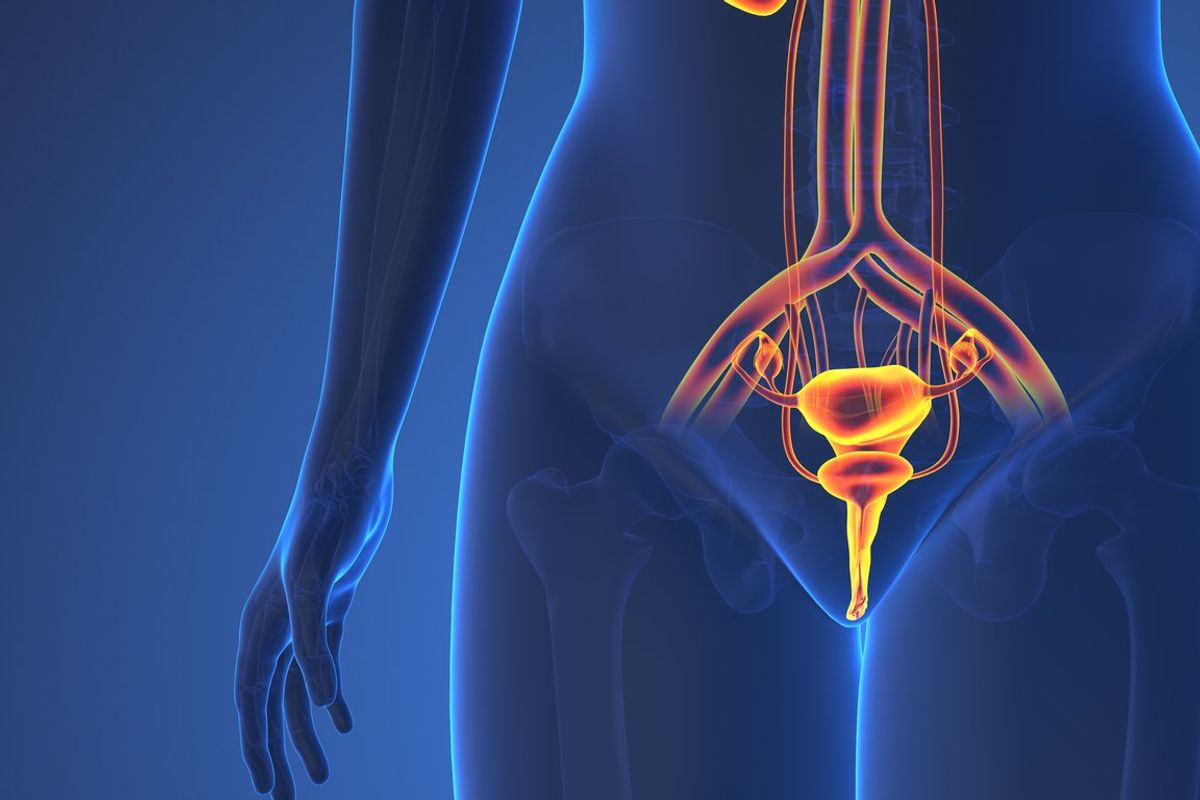
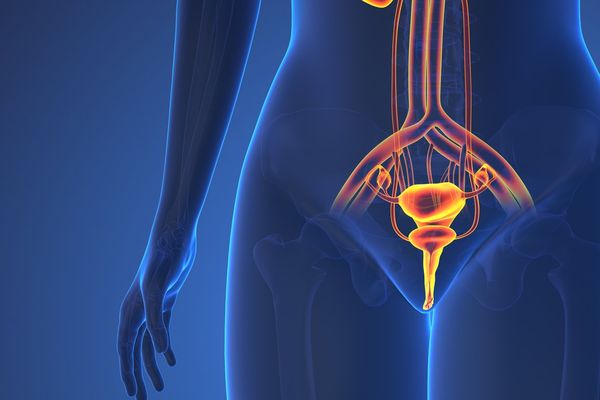
Given that your bladder is close to your reproductive organs, you may wonder how those organs might be affected if you have bladder cancer.
HealthyWomen spoke with two experts to get answers to the most frequently asked questions about taking care of your reproductive health when you have bladder cancer.
Lee A. Richter, M.D., is a board-certified urologist and associate professor of both urology and obstetrics and gynecology at Georgetown University School of Medicine. Melissa Donohue, DSW, is a licensed clinical social worker and certified sex therapist.
Can bladder cancer spread to my reproductive organs?
If you have bladder cancer, it means cancer cells are present in the bladder. Most of the time, the cancer stays inside the bladder, but in some instances, it leaves the lining of the bladder and spreads into or outside the muscle. This is known as muscle-invasive bladder cancer. And it’s rare, but possible, that this cancer can spread to your reproductive organs.
Does being in menopause increase my risk of bladder cancer?
There is some evidence that seems to suggest that the risk of bladder cancer goes up when menopause happens at an early age, but the data isn’t strong enough to say for sure. There also isn’t enough evidence to show that hormones, like estrogen, cause bladder cancer.
However, your chances of having bladder cancer increase with age. Menopause is a hormonal change, so even though there isn’t enough evidence to say menopause increases the risk, people who are postmenopausal are at higher risk for bladder cancer compared to premenopausal people.
Can being in perimenopause or menopause make it harder to get a diagnosis?
Blood in the urine is a major symptom of bladder cancer. So, if you’re in perimenopause and still getting periods, it may be hard to tell where the blood is coming from. Being in menopause also increases your risk of getting UTIs (because of lower estrogen levels), and UTIs are another reason for having blood in your urine. Your healthcare provider (HCP) may want to make sure the blood is not from one of these other causes before screening for cancer.
But, while your HCP is following their protocols for checking out blood in the urine, bladder cancer could spread and be more advanced by the time it’s caught.
If you’re tested for a UTI and get a negative result, it’s important to follow up with your HCP to see what’s causing blood in your urine. Bladder cancer and UTIs can also happen at the same time, so if you are diagnosed with a UTI and suspect something else is wrong, it’s OK to request further testing.
Read: For Nearly a Year, Doctors Dismissed My Bladder Cancer Symptoms as UTIs >>
Can I remain on birth control during cancer treatment?
You can continue using both hormonal and nonhormonal birth control even if you have bladder cancer. Bladder cancer doesn’t use hormones to grow and spread, so hormonal birth control, such as the pill or a hormonal intrauterine device (IUD), is safe to use. Non-hormonal birth control methods, such as the copper IUD, spermicide and condoms, are also safe.
Will treatment for bladder cancer suppress my period?
If you have surgery for bladder cancer that removes the uterus, fallopian tubes and ovaries, this can put you into menopause early and your period will stop. Some chemotherapy medications can also cause a temporary loss of your period.
Will bladder cancer treatment affect my fertility?
Because bladder cancer rarely affects the reproductive organs, bladder cancer treatment doesn’t usually involve removing the uterus or ovaries. There is a procedure called a genital-sparing cystectomy, which removes the bladder, but leaves the uterus and ovaries in place.
There’s a type of therapy known as neoadjuvant chemotherapy, which is chemotherapy that’s given before a cystectomy surgery to reduce and control cancer size and spread before the surgeon removes the cancer and bladder.
If you have to have this type of chemo, you won’t be able to become pregnant in the future and can develop menopausal symptoms such as hot flashes or vaginal dryness.
How can bladder cancer treatment affect my sex life?
Chemotherapy can cause vaginal dryness, which can lead to irritation. It can also cause mouth sores, making kissing and intimacy more difficult. You also might feel nausea or fatigue, which can make it hard to want to have sex.
Bladder surgery might also leave you with a urostomy bag, which is a pouch that collects urine outside your body. For some people, this can make them feel self-conscious with their partner. Sometimes, part of the vagina needs to be removed and this can shorten or narrow the vaginal canal, making intercourse uncomfortable, more difficult, or in some cases, impossible.
Communication, patience and compassion are key components for every couple. It can help to create new patterns, find your new normal, and redefine what sex is to you and your partner.
Will bladder cancer treatment affect perimenopause symptoms?
If you have chemotherapy as part of your bladder cancer treatment, you might have side effects such as hot flashes and vaginal dryness. Chemotherapy can also cause decreased sex drive and mood changes.
All of these can also be symptoms of perimenopause, so if you experience them currently, treatment could make them more intense.
Resources
Bladder Cancer Advocacy Network
This educational resource was created with support from Astellas and Pfizer.
- Bladder Cancer Survivors and Second Cancers - HealthyWomen ›
- Los sobrevivientes de cáncer de vejiga y los segundos cánceres primarios - HealthyWomen ›
- Mental Health and Urothelial Bladder Cancer - HealthyWomen ›
- Una buena nutrición y el cáncer de vejiga - HealthyWomen ›
- Good Nutrition and Bladder Cancer - HealthyWomen ›
- Bladder Cancer and Black Women - HealthyWomen ›
- El cáncer de vejiga y las mujeres de raza negra - HealthyWomen ›
- How to Regain Intimacy When Your Partner Has Bladder Cancer - HealthyWomen ›
- Cómo recuperar la intimidad cuando tu pareja tiene cáncer de vejiga - HealthyWomen ›