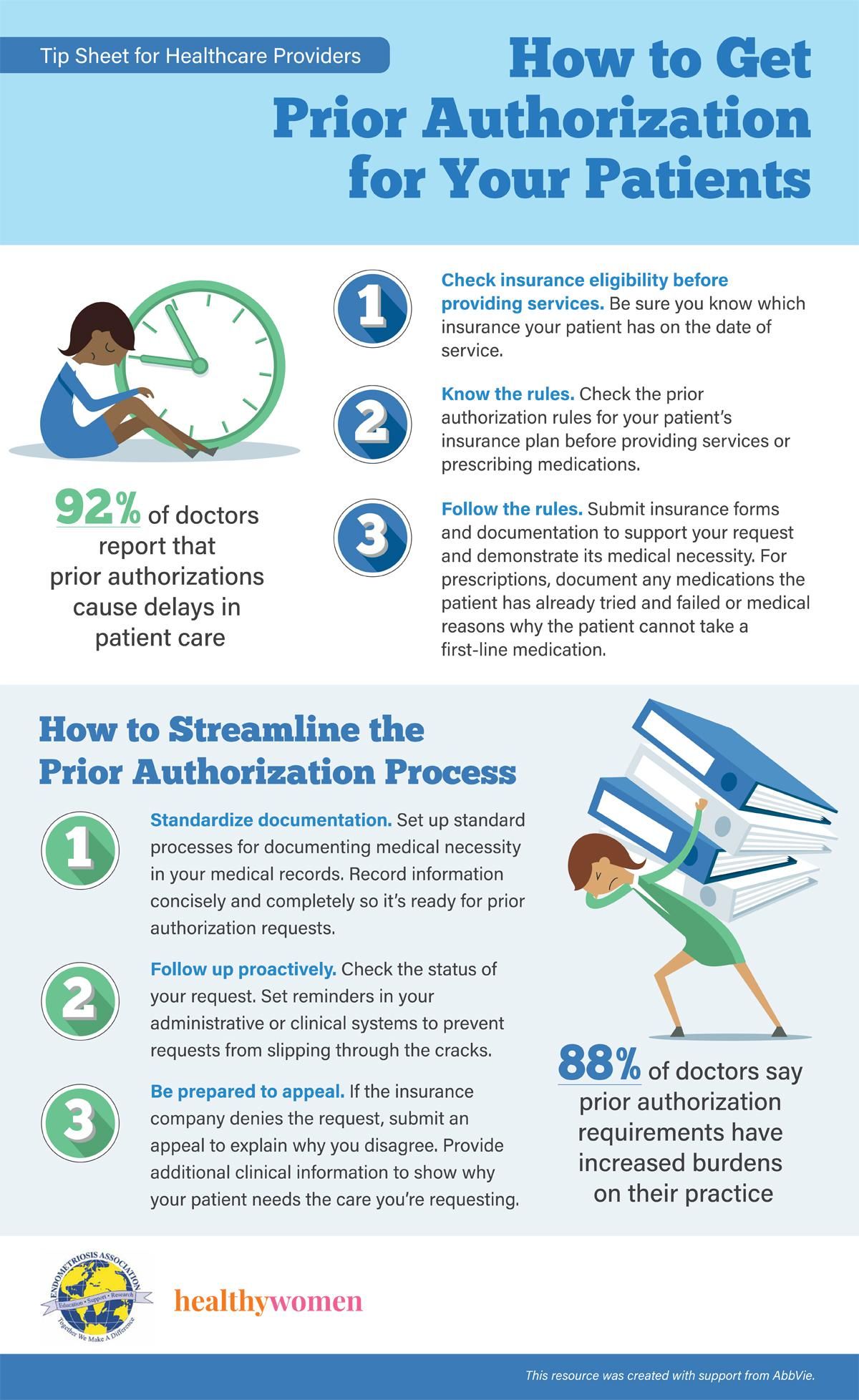
Check insurance eligibility before providing services. Be sure you know which insurance your patient has on the date of service.
Know the rules. Check the prior authorization rules for your patient’s insurance plan before providing services or prescribing medications.
Follow the rules. Submit insurance forms and documentation to support your request and demonstrate its medical necessity. For prescriptions, document any medications the patient has already tried and failed or medical reasons why the patient cannot take a first-line medication.
92% of doctors report that prior authorizations cause delays in patient care.
How to Streamline the Prior Authorization Process
Standardize documentation. Set up standard processes for documenting medical necessity in your medical records. Record information concisely and completely so it’s ready for prior authorization requests.
Follow up proactively. Check the status of your request. Set reminders in your administrative or clinical systems to prevent requests from slipping through the cracks.
Be prepared to appeal. If the insurance company denies the request, submit an appeal to explain why you disagree. Provide additional clinical information to show why your patient needs the care you’re requesting.
88% of doctors say prior authorization requirements have increased burdens on their practice
Source: American Medical Association. “Tips to help physicians reduce the prior authorization burden in their practice.”
This resource was created with support from AbbVie.