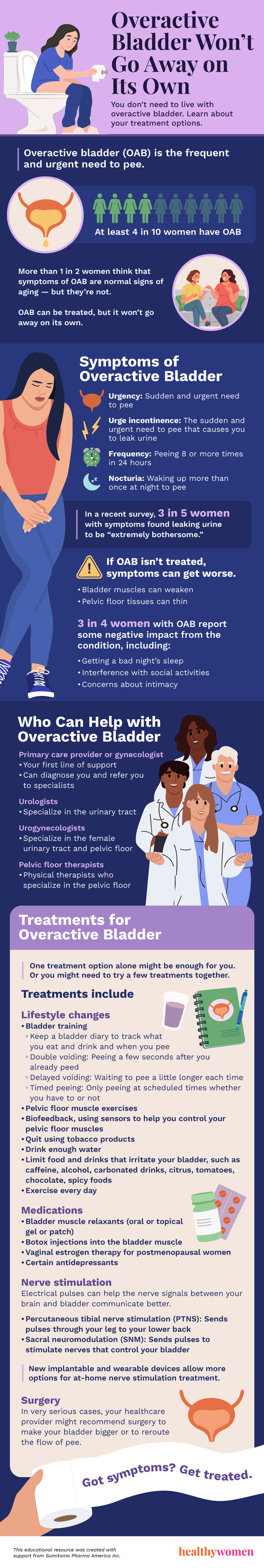
Overactive bladder (OAB) is the frequent and urgent need to pee.
At least 4 in 10 women have OAB.
More than 1 in 2 women think that symptoms of OAB are normal signs of aging — but they’re not.
OAB can be treated, but it won’t go away on its own.
Symptoms of Overactive Bladder
- Urgency: Sudden and urgent need to pee
- Urge incontinence: The sudden and urgent need to pee that causes you to leak urine
- Frequency: Peeing 8 or more times in 24 hours
- Nocturia: Waking up more than once at night to pee In a recent survey, 3 in 5 women with symptoms found leaking urine to be “extremely bothersome.”
If OAB isn’t treated, symptoms can get worse.
- Bladder muscles can weaken
- Pelvic floor tissues can thin
3 in 4 women with OAB report some negative impact from the condition, including:
Getting a bad night’s sleep
Interference with social activities
Concerns about intimacy
Who Can Help with Overactive Bladder
Primary care provider or gynecologist
- Your first line of support
- Can diagnose you and refer you to specialists
Urologists
- Specialize in the urinary tract
Urogynecologists
- Specialize in the female urinary tract and pelvic floor
Pelvic floor therapists
- Physical therapists who specialize in the pelvic floor
Treatments for Overactive Bladder
One treatment option alone might be enough for you. Or you might need to try a few treatments together.
Treatments include
Lifestyle changes
- Bladder training
- Keep a bladder diary
- Track what you eat and drink and when you have the urge to pee
- Double voiding
- Peeing again a few seconds after you already peed
- Delayed voiding
- Waiting to pee a little longer each time
- Timed peeing
- Only peeing at certain scheduled times whether you have to or not
- Pelvic floor muscle exercises
- Biofeedback, using sensors to help you control your pelvic floor muscles
- Quit using tobacco products
- Adjust your diet
- Drink enough water
- Limit food and drinks that irritate your bladder
- Caffeine, alcohol, carbonated drinks, acidic foods like citrus or tomatoes, chocolate, spicy foods
- Exercise every day
Medications
- Bladder muscle relaxants
- Can be taken by mouth or applied to the skin through gel or patch
- Botox
- Injections into the bladder muscle help it relax
- Vaginal estrogen therapy for postmenopausal women
- Certain antidepressants
Nerve stimulation
Electrical pulses can help the nerve signals between your brain and bladder communicate better.
- Percutaneous tibial nerve stimulation (PTNS)
- Sends pulses through your leg to your lower back
- Sacral neuromodulation (SNM)
- Sends mild electric impulses to stimulate nerves that control your bladder
New implantable and wearable devices allow more options for at-home nerve stimulation treatment.
Surgery
In very serious cases, your healthcare provider might recommend surgery to make your bladder bigger or to reroute the flow of pee.
Got symptoms? Get treated.
This educational resource was created with support from Sumitomo Pharma America Inc.