It’s hard enough finding time to get together with our girlfriends between family responsibilities, work and (trying to) squeeze in a workout. We shouldn’t let the anxiety of making sure there’s always a bathroom around stop us from finally getting in those much needed laughs. For 33 million U.S. adults — and 4 out of 10 women — that anxiety is real. The culprit? Overactive bladder (OAB).
OAB is the sudden and urgent feeling that you need to pee even when your bladder isn’t full. OAB is common. And more than 1 in 3 of those with OAB also experience urinary urge incontinence — when you have a sudden and urgent need to pee that you cannot stop.
OAB often occurs in people over age 65, but women often experience it earlier, in their 40s. In a recent study conducted by HealthyWomen, 3 out of 4 women with OAB reported that they experienced some sort of negative impact from living with the condition, including getting a poor night’s sleep, worrying about where they might be able to find bathrooms during social activities and having concerns about intimacy.
In that same study, more than 1 in 2 women reported that they thought symptoms of OAB were just a normal part of aging, but they’re not. OAB is a medical condition that can be managed by treating the symptoms and making certain lifestyle changes.
Here’s what you need to know about OAB so you can get the treatment you deserve — and turn off that bathroom radar.
What are the symptoms of OAB?
Symptoms of OAB include:
- The sudden urge to pee even if you just went, which can sometimes result in leaking urine (called urinary urge incontinence).
- Peeing more than eight times in 24 hours.
- Nocturia, or getting up to pee at night more than once.
How does a healthy bladder work?
iStock.com/MatoomMi
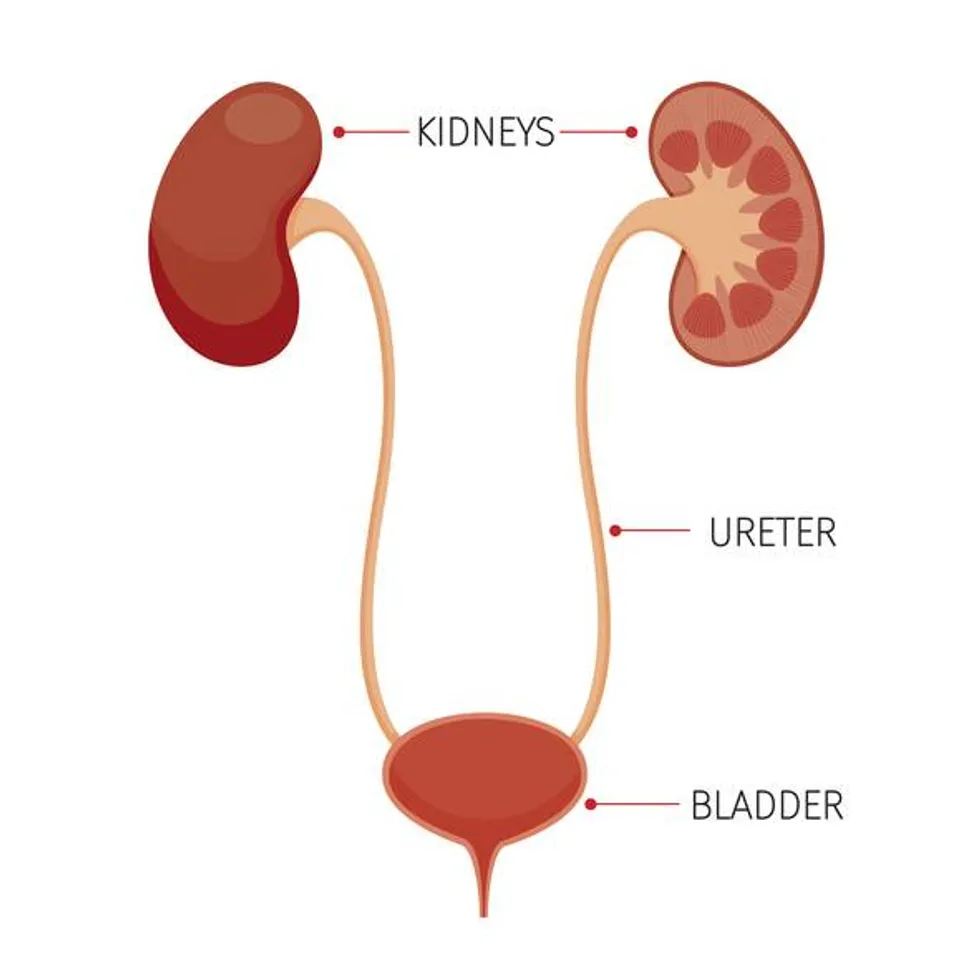
The bladder is part of the urinary tract. The urinary tract also includes two kidneys, two ureters, a urethra and internal and external sphincter muscles.
Your kidneys filter blood to remove waste in the form of pee. While the kidneys are working to fill your bladder with pee, your bladder muscles stay relaxed and your sphincter muscles stay tight and closed. When you need to pee, your brain sends a signal to the sphincters to relax and then tells the bladder muscles to tighten so it can squeeze pee through the urethra and out of the bladder.
What causes OAB?
Researchers don’t know the exact cause of OAB. But there are a few different factors that may be behind it.
When you don’t have OAB, your brain receives a signal that it’s time to go to the bathroom once the bladder fills up. But when you have OAB, your brain receives the signal before the bladder is full and the muscles contract, signaling that it’s time to go.
Sometimes the bladder muscles tighten on their own. This is called involuntary bladder contractions or bladder spasms. When spasms happen, your bladder squeezes out the urine it's holding, which can cause a sudden, urgent need to pee or even leakage. Some reasons your bladder may spasm include neurological conditions, inflammation or obstructions like pelvic organ prolapse or kidney stones.
Certain neurological conditions like Parkinson’s disease or multiple sclerosis (MS) affect the body’s ability to control its nervous system and regular functions. These conditions can interfere with the brain’s connection to the bladder and can cause OAB. Other bodily traumas such as nerve damage, injuries to the belly or lower back area, or infections like urinary tract infections (UTIs) can increase OAB symptoms. Having overweight or obesity also increases the risk of OAB from extra pressure pushing on the bladder.
Sometimes medications are the cause of OAB. Diuretics, or water pills, that are used to treat high blood pressure and fluid retention can cause the bladder to fill up more frequently than usual. Alpha blockers that treat high blood pressure can relax the bladder muscles, which makes pee flow more easily and increases feelings of urgency.
OAB might also be caused by certain lifestyle factors like drinking caffeine or alcohol; smoking; or eating certain foods like acidic food, spicy food or artificial sweeteners. Both drinking too much or too little water can cause OAB by irritating the bladder. Balance is important — women should aim for about nine cups of fluids a day plus the fluids that naturally come from eating food. Constipation can also increase OAB symptoms.
During perimenopause and menopause, your body decreases the amount of the hormone estrogen it produces. This can weaken the pelvic floor muscles and lead to OAB. The effects can be even greater if you’ve delivered a baby because childbirth — both vaginally and by cesarean section — can also weaken pelvic floor muscles. OAB can also result when the weakened pelvic floor muscles lead to pelvic organ prolapse.
The link between OAB and cognitive decline
Cognitive decline is the decreased ability to think, learn, remember, use judgement and make decisions. Although research has shown that people with OAB, particularly women, tend to have lower cognitive health than those without it, researchers don’t yet know why. One theory is that the decline may be the result of poor quality of sleep from waking up to pee at night.
In addition, depression, which is a known risk factor for cognitive decline, has also been associated with OAB. People with OAB may have signs of depression because of the way OAB can affect sleep as well as your lifestyle and social interactions. However, the relationship is still unclear, and some studies also suggest that OAB may be one of the early signs of cognitive decline or dementia.
When is it time to see a healthcare provider?
OAB won’t go away on its own. There are several different treatments available that can help including lifestyle changes, medications, nerve stimulation and surgery.
If you’re experiencing any symptoms of OAB, you should talk to your healthcare provider about your options. Keeping a bladder diary that tracks what you eat and drink and how often you have the urge to pee can help guide the conversation with your medical team.
This educational resource was created with support from Sumitomo Pharma America.
- Need to Pee During Sex? How Overactive Bladder Affects Intimate Relationships ›
- I Didn’t Let Overactive Bladder Stop Me from Living My Life ›
- Overactive Bladder: Those Awkward Questions You Want and Need to Ask ›
- Overactive Bladder Can Affect Your Daily Life ›
- Overactive Bladder Symptoms You Should Share With Your Health Care Provider ›
- Treatments for Overactive Bladder - HealthyWomen ›







